Faculty Peer Reviewed
Blood transfusions are one of the most common interventions seen in the inpatient setting. While hanging a unit of blood appears simple enough in day-to-day practice, many of us forget what this simple action actually entails. Taking a moment to reflect, Clinical Correlations breaks down this basic, everyday intervention by the numbers.
How much blood are we transfusing?
In the United States, it is estimated that approximately 14.65 million units of whole blood/RBCs are transfused each year. Additionally, it is reported that 10.39 million units of platelets are transfused annually [1].
How much does this cost?
Previously, it was estimated that each unit of RBCs transfused cost $322. However, recent estimates suggest that the actual total cost (using an activity-based cost model) is far higher at $761 (± $294) per unit of RBCs. This newer estimate takes into account costs associated with acquiring, delivering, administering, and monitoring each transfusion [2].
How risky is this intervention?
Each time we counsel patients about the risks and benefits of a transfusion, it is imperative that we inform them about the possible complications and adverse events associated with receiving a transfusion. However, how often do we put these risks in terms of actual prevalence? Based on data collected in the U.S. in 2009, we find that the prevalence estimates of selected adverse events are [3]:
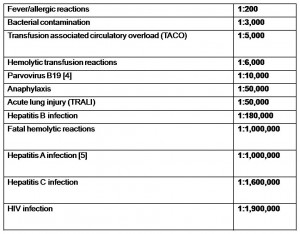 Moreover, recent studies have identified emerging (but rare) transfusion-related infectious risks including West Nile Virus (23 cases in 2002-2003), malaria (2-3 cases reported per year over the last 40 years), Chagas’ Disease (6 cases in North American since the mid-1980s), variant Creutzfeldt-Jakob Disease (129 cases reported in England), Epstein-Barr virus, leishmaniasis, Lyme disease, brucellosis, babesiosis, and toxoplasmosis [5,6].
Moreover, recent studies have identified emerging (but rare) transfusion-related infectious risks including West Nile Virus (23 cases in 2002-2003), malaria (2-3 cases reported per year over the last 40 years), Chagas’ Disease (6 cases in North American since the mid-1980s), variant Creutzfeldt-Jakob Disease (129 cases reported in England), Epstein-Barr virus, leishmaniasis, Lyme disease, brucellosis, babesiosis, and toxoplasmosis [5,6].
Do these numbers change the way we think about transfusions in everyday practice?
Looking at the numbers, some aspects of blood transfusions are not all that surprising. Particularly, the sheer number of transfusions administered in the United States is predictably high. However, some findings were unexpected and are perhaps worth keeping in mind in everyday practice. Specifically, the cost per unit of blood was much greater than expected, especially using estimates that take the total associated costs into account. While blood transfusions can be potentially lifesaving and certainly worth the expense, the cost is an interesting number to consider in the context of ever increasing hospital expenditures and the recent policy drive toward healthcare costs savings. Additionally, some of the actual risks from blood transfusions are surprising. While blood transfusions have become increasingly safe over time (as compared to the 50% mortality associated with the first reported transfusion in 1828 [7]), it is interesting how common bacterial contamination remains are with a prevalence of 1 in 3,000 units transfused. Notably, platelets carry the greatest risk of bacterial contamination as they are stored for up to 5 days at 68 – 75.2ï‚° F [5]. It surprising how common this risk is compared to the other more often discussed (but far less common) infectious risks, such as hepatitis or HIV.
Additionally, in bringing the discussion back to everyday practice, it is worthwhile to mention how indications for red cell transfusions in adults have changed over time. In the perioperative or intensive care unit setting, it is still unclear whether there is a specific optimal transfusion level. However, over the last twelve years, after the publication of the TRICC (Transfusion Requirements in Critical Care) trial, there has been increasing evidence to support a more restrictive transfusion strategy (transfusion at hemoglobin < 7 g/dL) as opposed to a more liberal transfusion strategy (transfusion at hemoglobin <10 g/dL) in this clinical setting. The TRICC trial found mortality rates were significantly lower in younger (< 55 years) and less severely ill patients (APACHE II score of ï‚£ 20) who were randomized to the restrictive transfusion arm of the study [8]. These findings along with later studies [9, 10, 11, 12] suggest that a restrictive transfusion threshold of a hemoglobin of 7 g/dL is at least as safe (and possibly superior depending on patient characteristics) as a more liberal threshold in transfusing critically ill patients with hemodynamically stable anemia.
Looking at transfusions by the numbers does not necessarily change the decision to hang a unit of blood, but rather, these numbers provide context about the intervention and importantly, more information to offer patients when providing informed consent for a transfusion.
Dr. Karen Chang Kan is a resident at NYU Langone Medical Center
Peer reviewed by Neil Shapiro, Editor-In-Chief, Clinical Correlations
References:
[1] . Whitaker BI, Green J, King MR, Leibeg LL, Mathew SM, Schlumpf KS, Schreiber GB. 2007 National blood collection and utilization survey. Bethesda (MD): Dept. of Health and Human Services (US); 2007
[2] Shander A, Hofmann A, Ozawa S, Theusinger OM, Gombotz H, Spahn DR. Activity-based costs of blood transfusions in surgical patients at four hospitals. Transfusion. 2010 Apr; 50(4): 753-65. http://onlinelibrary.wiley.com/doi/10.1111/j.1537-2995.2009.02518.x/abstract
[3] Klein HG. How safe is blood, really? Biologicals. 2010 Jan 15; 38(1): 100-4. http://www.sciencedirect.com/science?_ob=ArticleURL&_udi=B6WBS-4Y5H62J-1&_user=10&_coverDate=01%2F31%2F2010&_alid=1740848539&_rdoc=1&_fmt=high&_orig=search&_origin=search&_zone=rslt_list_item&_cdi=6718&_sort=r&_st=13&_docanchor=&view=c&_ct=2&_acct=C000050221&_version=1&_urlVersion=0&_userid=10&md5=67ad71cd504f4d05359957b7b12ac42c&searchtype=a
[4] Goodnough LT, Brecher ME, Kanter MH, AuBuchon JP. Transfusion medicine. N Engl J Med. 1999 Feb 11; 340(6): 438-47. http://www.nejm.org/doi/full/10.1056/NEJM199902113400606
[5] Goodnough LT. Risks of blood transfusion. Anesthesiology Clin N Am. 2005 May 26; 23(2): 241-52. http://www.sciencedirect.com/science?_ob=ArticleURL&_udi=B75HC-4G82R51-5&_user=10&_coverDate=06%2F30%2F2005&_rdoc=1&_fmt=high&_orig=gateway&_origin=gateway&_sort=d&_docanchor=&view=c&_searchStrId=1741852218&_rerunOrigin=google&_acct=C000050221&_version=1&_urlVersion=0&_userid=10&md5=903eca6df91759ba815de6f55468c1ba&searchtype=a
[6] Busch MP, Kleinman SH. Current and emerging infectious risks of blood transfusions. JAMA. 2003 Feb 26; 289(8): 959-62. http://jama.ama-assn.org/content/289/8/959.short
[7] Blundell J. Observations on the transfusion of blood. Lancet 1828; 2(ii): 321-4. http://woodlibrarymuseum.org/rarebooks/item/129/blundell-j.-observations-on-transfusion-of-blood,-with-a-description-of-his-gravitator,-1828-29.
[8] Hebert PC, Wells G, Blajchman MA, et al. A multicenter, randomized, controlled clinical trial of transfusion requirements in critical care. N Engl J Med 1999; 340-409. http://www.ncbi.nlm.nih.gov/pubmed/9971864
[9] Bracey AW, Radovancevic R, Riggs SA, et al. Lowering the hemoglobin threshold for transfusion in coronary artery bypass procedures: effect on patient outcome. Transfusion 1999; 39:1070.
[10] Corwin HL, Gettinger A, Pearl RG, et al. The CRIT Study: anemia and blood transfusion in the critically ill – current clinical practice in the United States. Crit Care Med 2004; 32: 39-52.
[11] Palmieri TL, Caruso DM, Foster KN, et al. Effect of blood transfuion on outcome after major burn injury: a multicenter study. Crit Care Med 2006; 34: 1602-7.
[12] Marik PE, Corwin HL. Efficacy of red blood cell transfusion in the critically ill: a systematic review of the literature. Crit Care Med


2 comments on “Transfusions By The Numbers”
Very nice review, Karen, reminding us that with transfusions, as in many areas of medical practice, a conservative approach may well be the safest one for the patient.
I’ve always felt that transfusion of patients based on H/H levels is usually inappropriate, but the decision to transfuse should be based on hemodynamic ad physiologic responses by the patient, risks for complications of severe anemia like cardiovascular disease, etc. The indications for transfusion or not are specific to each clinical situation.
Comments are closed.