Faculty Peer Reviewed
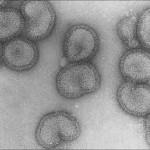
Flu season is upon us. According to the CDC, flu outbreaks start as soon as October and usually end in May, with a peak around February. Vaccinations for the general public typically begin in September with a focus on high-risk groups, including the young, the old, and those who are immunocompromised [1]. However, few know of the origins of vaccinations. Long gone are the days where freshly dried small pox scabs were ground into dust and administered by “nasal insufflation.†Arguably, vaccine administration is not as barbaric as it was in the past.
Whether or not it should be mandatory for all healthcare workers to be immunized is highly debatable. Proponents argue it is not just for the health of the workers, but also to reduce transmission to patients. Opponents include those who believe the vaccine carries certain unnecessary risks, such as Guillain-Barré or poor efficacy [2]. In particular, recent literature has addressed the development of Guillain-Barré. In trying to convince patients to accept the vaccine, new evidence is mounting showing a lack of association between the flu vaccine and Guillain-Barré Syndrome. In a case-centered study published in Clinical Infectious Diseases, the authors identified a total of 415 cases of hospitalized Guillain-Barré Syndrome patients from 1995 to 2006 at Kaiser Permanente Northern California. Each case was reviewed by a neurologist. Unclear diagnoses of Guillain-Barré Syndrome, Miller-Fisher variants, and chronic inflammatory demyelinating polyradiculoneuropathy were excluded. All patients analyzed were exposed to vaccinations within one year, with influenza having a limit of nine months. The odds of vaccination were compared in the prior 6- and 10-week interval in all Guillain-Barré syndrome-affected patients and in all vaccinated individuals in the entire center population. The authors found no increased risk of Guillain-Barré Syndrome following vaccinations of any kind [3]. Interestingly enough, a new study in the Lancet Infectious Diseases by Kwong et al. found that the risk of Guillain-Barré Syndrome was higher in those who were infected with influenza than those who were vaccinated, as previously mentioned in an earlier post in Primecuts. In short, the authors estimated the attributable risk of Guillain-Barré Syndrome to be 1.03 admissions per million vaccinations and 17.2 admissions per million for influenza-coded health-care encounters. While relatively small numbers, this study added to a growing body of evidence that the risk of Guillain-Barré Syndrome is significantly higher in those who develop influenza when compared to those who are vaccinated [4]. Though the influenza vaccine may indeed carry an increased risk of Guillain-Barré Syndrome (albeit small), those infected by the influenza virus carry an even higher risk.
In other vaccination news, a recent paper in Nature shows a possible candidate for an HIV vaccine. Hansen et al. developed a vaccine using a CMV vector expressing Simian Immunodeficiency Virus (SIV) proteins. His team vaccinated 16 rhesus monkeys, then later inoculated them with a highly pathogenic strain of SIV. All of the monkeys showed an initial viremia and signs of infection in the first few weeks. By 40 weeks, 9 of the 16 who survived all showed undetectable levels of the virus. The control group, composed of 18 rhesus monkeys, all showed no evidence of viremic control. While this vaccine did not prevent SIV infection, evidence shows that it helped to sequester the virus by limiting it mostly to the bone marrow and preventing or limiting spread to peripheral lymph nodes and small intestinal mucosa. Obviously there are hurdles to overcome, including increasing the number of responders and translating the SIV vaccine in rhesus monkeys to an HIV vaccine in humans. While this vaccine may not be preventative, it may serve as a model for a therapeutic vaccine in the future [5].
And speaking of injections, a new study on methylprednisolone injections for those with primary idiopathic carpal tunnel was recently published in the Annals of Internal Medicine. In a double blind, randomized placebo controlled trial, three groups of 37 patients ages 18-70 who failed wrist splinting were randomized to either 80mg methylprenisolone, 40mg methylprednisolone, or placebo injections. These patients were followed up at 10-weeks for symptom severity and at 1-year for the rate of surgery. The decision for surgery was solely decided upon by the patient. There was a statistically significant improvement in symptom severity in the methylprednisolone groups vs. the placebo group. No difference was found between the 40mg and the 80mg groups. At one year, only the 80mg methylprednisolone group had a statistically significant decrease in rate of surgery (73%, P = 0.042). The 40mg group and placebo group had a 1-year surgery rate of 81% and 92%, respectively. In summary, in patients who have carpal tunnel syndrome and who have failed wrist splinting, methylprednisolone injection significantly decreases symptom severity at 10 weeks but has a minimal impact on the rate of surgery at 1 year [6]. Based on these findings, patients with carpal tunnel syndrome who have failed splinting should have a trial of corticosteroid injection therapy. However, corticosteroids are probably a short term treatment and patients will most likely require surgery in the future.
Again shifting gears but still following the theme of injections, we take a look at a different kind of steroid. Feeling fatigued? Depressed? Have a low libido? Perhaps low testosterone (otherwise marketed as “Low Tâ€) is to blame. Clinically, low testosterone is measured by having a testosterone level two standard deviations below the mean. Finkelstein et al. looked at testosterone and estradiol levels in men and how their levels affected percent body fat, subcutaneous fat, intra-abdominal fat, thigh muscle area and strength, and sexual function. In this study, men ages 20-50 had their endogenous testosterone production suppressed by the administration of goserelin acetate, a gonadal releasing hormone (GnRH) agonist. In some men, anastrozole, an aromatase inhibitor, was also given to suppress the conversion of testosterone to estradiol, effectively suppressing endogenous estradiol production. In general, lower levels of testosterone resulted in higher percentage of body fat, and a lower lean mass. Libido decreased in a near stepwise fashion and erectile dysfunction varied through all the different interventions. Though this was a study within a limited time period, marked clinical changes related to sex hormone levels were apparent in the study subjects. Not all were dose-dependent, indicating that testosterone deficiency should be based on a more individual-tailored approach instead of a standard laboratory value. Estradiol may also play a role in some of the symptoms associated with low testosterone, including sexual dysfunction, bone loss, or body fat and exerted effects independent from those of testosterone [7]. Perhaps we should consider checking estradiol levels in a patient who presents with symptoms of low testosterone.
Other interesting reads:
1. Planche TD, et al. Differences in outcome according to Clostridium difficile testing method: a prospective multicentre diagnostic validation study of C difficile infection. The Lancet Infectious Diseases. 3 September 2013. DOI: 10.1016/S1473-3099(13)70200-7 Epub ahead of print. http://www.thelancet.com/journals/laninf/article/PIIS1473-3099(13)70200-7/fulltext
Do the results of different C. diff laboratory tests affect mortality? In this study, it did. In unformed stool samples submitted for routine C. diff testing in the UK, a positive C. diff toxin was found to correlate more positively with true cases of C. diff (and consequently, higher rates of mortality), whereas a positive cytotoxigenic culture (glutamate dehydrogenase) without evidence of the toxin did not. They bring up the idea of a C. diff excretor (otherwise known as a colonized person), where isolation may be necessary to prevent cross-infection, but treatment may not be indicated.
2. Reed M, Huang J, Brand R, et al. Implementation of an Outpatient Electronic Health Record and Emergency Department Visits, Hospitalizations, and Office Visits Among Patients With Diabetes. JAMA. 2013;310(10):1060-1065. doi:10.1001/jama.2013.276733. http://jama.jamanetwork.com/article.aspx?articleid=1737043&resultClick=3
This study adds to the limited amount of data available regarding the use of an electronic health record (EHR) to improve patient outcomes. The use of an EHR was associated with a statistically significant decrease in ED visits and fewer hospitalizations in diabetic patients located in Northern California.
3. Nicholls SJ, Bakris GL, Kastelein JP, et al. Effect of Aliskiren on Progression of Coronary Disease in Patients With Prehypertension: The AQUARIUS Randomized Clinical Trial. JAMA. 2013;():-. doi:10.1001/jama.2013.277169. http://jama.jamanetwork.com/article.aspx?articleid=1734674&resultClick=3
In this double blinded, randomized, multicenter trial looking at patients with coronary artery disease, prehypertension, and two additional risk factors, subjects were evaluated using coronary intravascular ultrasound, given aliskiren or placebo for two years, then reevaluated. Although a statistically significant decrease in blood pressure was noted, no improvement or slowing of progression of coronary atherosclerosis was observed.
Brian Yuen, MD is a first-year internal medicine resident at NYU Langone Medical Center
Peer Reviewed by Matthew Vorsanger, MD, Associate Editor, Clinical Correlations
References:
1. Centers for Disease Control and Prevention. What you should know about the 2013-2014 influenza season. http://www.cdc.gov/flu/about/season/flu-season-2013-2014.htm
2. Schonberger LB, et al. Guillain-Barre Syndrome Following Vaccination in the National Influenza Immunization Program. United States. 1976-1977. American Journal of Epidemiology. 110(2): 105-123.
3. Baxter R, et al. Lack of association of Guillain-Barre syndrome with vaccinations. Clin Infect Dis 57(2): 197-204.
4. Kwong JC, Vasa PP, Campitelli MA, et al. Risk of Guillain-Barré syndrome after seasonal influenza vaccination and influenza health-care encounters: a self-controlled study. Lancet Infectious Disease. 2013 Sep;13(9):769-76.
5. Hansen SG, et al. Immune clearance of highly pathogenic SIV infection. Nature. doi: 10.1038/nature12519. [Epub ahead of print]
6. Atroshi I, Flondell M, Hofer M, Ranstam J. Methylprednisolone Injections for the Carpal Tunnel SyndromeA Randomized, Placebo-Controlled Trial. Annals of Internal Medicine. 2013 Sep;159(5):309-317.
7. Finkelstein JS, et al. Gonadal Steroids and Body Composition, Strength, and Sexual Function in Men. New England Journal of Medicine 369(11): 1011-1022.