By David Kudlowitz, MD
Faculty Peer Reviewed
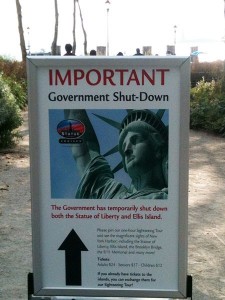
For the first time since 1996, the government has shut down due to lack of Congressional funding. Most of the wrangling behind this political stalemate surrounds support of the Affordable Care Act. Meanwhile, 800,000 non-essential federal employees are out of work and various services are offline. While legislators continue to argue over the politics of health care reform, the Affordable Care Act’s online health exchanges opened on October 1. In other news, at the United Nations, Israeli Prime Minister Benjamin Netanyahu stated Iran’s new president Hassan Rouhani is a “wolf in sheep’s clothing†with regards to nuclear weapons, Microsoft’s investors want Bill Gates to step down as chairman, and AMC’s Breaking Bad had its series finale, which was widely lauded and had over 10 million viewers. In the the world of medicine this week, there were a number of notable articles published that can be found on PubMed for further review, although keep in mind the site is running on minimal staffing due to lack of funding.
First up, in a meta-epidemiological study in the BMJ, authors looked to compare the effectiveness of exercise and pharmacologic intervention on mortality reduction in the therapy of several common diseases [1]. Researchers reviewed 16 meta-analyses, which included more than 300 trials and 300,000 participants from the last 14 years. Four meta analyses were identified with evidence supporting the effectiveness of exercise in the secondary prevention of coronary heart disease, treatment of heart failure, rehabilitation of stroke, and prevention of diabetes. In each of these disease states, exercise was found to have a significant effect on mortality. The additional 12 meta-analyses included trials in which patients received standard drug therapies for the treatment of the same diseases, according to clinical practice guidelines. Comparison was performed using network meta-analysis which generalizes the differences between paired meta-analyses, given the paucity of head to head trials in this investigation. Analysis of heterogeneity among the trials included in the study was also performed. Patient groups had comparable baseline characteristic with the exception of patients with stroke. Those who received pharmacologic therapy for cerebral infarction were within two weeks of the stroke whereas the exercise groups were able to participate up to 150 days after the event.
Key findings of the study were as follows; upon comparison of patients with coronary artery disease, there were no significant differences in mortality among statins, b blockers, ACE inhibitors, antiplatelet agents and exercise. In stroke, mortality with exercise was significantly lower than with anticoagulants or antiplatelet agents, although the pooled number of events was low in the exercise studies. In patient’s with heart failure, diuretics significantly lowered odds of mortality more than exercise, ACE inhibitors, angiotensin receptor blockers, and b blockers. For patients with pre-diabetes, neither medications nor exercise significantly reduced mortality.
The results of these pooled meta-analyses suggest that exercise has similar effects on mortality in coronary disease and superior effects on mortality in stroke when compared to medical therapy, however patients should not throw away their pills just quite yet. Exercise was poorly and variably defined in these studies and there are limited trials directly comparing exercise versus medical therapy in the secondary prevention of these common diseases. The studies included in this investigation were fairly heterogeneous and for the disease state with the most positive outcome (stroke), the patients included were markedly different at baseline. The results of the heart failure meta analyses were also contradictory to current evidence, with diuretic therapy demonstrating more efficacy than beta blockers. With pharmacologic therapy increasingly relied upon by an aging population, exercise can be an important and cost-effective manner of impacting disease, although more trials, with direct comparisons, are needed to draw any significant conclusions.
JAMA published a study this week that examined opioid use in patients before and after bariatric surgery, with some unexpected results. As a result of multiple chronic pain issues associated with obesity, patients are prescribed opioids, despite a lack of long-term efficacy and previously demonstrated increased mortality [2], [3]. This retrospective cohort study, looked at 11,719 bariatric surgery patients across ten hospitals in the United States. Of those patients, 8% were chronic opioid users prior to surgery. One year after surgery, 77% of those patients continued chronic opioid use. The amount used, in total daily morphine equivalents, actually increased from pre-op 45 mg (95% CI, 40.0-50.1) to post-op 51.9 mg (95% CI, 46.0-57.8, p < 0.001) [4]. This increase in opioid use did not correlate with the degree of weight loss, depression, or preoperative diagnoses associated with chronic pain. Investigators had hypothesized that pain was linked to a patient’s obesity, and expected opioid use to decrease after bariatric surgery with subsequent weight loss. The results of this study suggest, however, that bariatric patients may have pain unresponsive to operative intervention. Alternatively, this study may be emblematic of a larger problem; that patients and physicians have great difficulty terminating opioid use for chronic pain.
In the NEJM this week, saxagliptin and alogliptin, two dipeptidyl peptidase 4 (DPP-4) inhibitors were evaluated in double blind, randomized controlled trials comparing cardiovascular outcomes. These studies are especially important because thus far, metformin and insulin are the only two medications with proven cardiovascular benefit, and in the case of older sulfonylureas and thiazolidinediones, there is an increased risk of death and heart failure [5],[6].
The first study evaluated saxagliptin vs. placebo in 16,492 patients with Type 2 Diabetes [7]. Eligibility factors included a history of one established cardiovascular disease risk factor or multiple cardiovascular risk factors and patients with end stage renal disease were excluded. Patients were randomized to either saxagliptin (dose based on GFR) or placebo, however could receive additional anti-hyperglycemics at their primary care providers discretion during a median follow up of 2.1 years. Primary end-point was composite of cardiovascular death, non-fatal myocardial infarction, or non-fatal stroke with analysis performed according to intention to treat. This end-point was seen in 7.3% saxagliptin patients and (7.2%) in those receiving placebo (hazard ratio 1.00; 95% CI 0.89 to 1.12; P=0.99 for superiority). Notably, more patients randomized to saxagliptin were hospitalized for heart failure (3.5% vs. 2.8%, p=0.007) and experienced major hypoglycemic events (2.1% vs. 1.7%, p=0.047).
The second study is a randomized, controlled, double-blind noninferiority trial evaluating alogliptin vs. placebo in 5380 patients with type 2 diabetes [8]. All patients were diagnosed with acute myocardial infarction or unstable angina requiring hospitalization within 15-90 days of the study. Patients were randomized to receive either alogliptin (dose based on GFR) or placebo in a 1:1 ratio. Patients were continued on any previously prescribed antihyperglycemic and cardiovascular agents. Those patients requiring hemodialysis in the previous 14 days, with NYHA class IV heart failure, uncontrolled arrhythmias, hypertension, or critical valvular disease were excluded. The primary end point was composite death due to cardiovascular cause, nonfatal myocardial infarction, or nonfatal stroke. The primary endpoint was seen in 11.3% of alogliptin patients and 11.8% of the placebo group at 18 months (hazard ratio 0.96; P<0.001 for noninferiority, P=0.32 for superiority). There was no comment on hospitalization for heart failure and there was no difference in episodes of major hypoglycemia between the two groups.
Traditionally, the macrovascular complications of diabetes have been difficult to prevent. The patient cohorts examined in these trials were both at high cardiovascular risk, however there were crucial differences between these two investigations. The saxagliptin study focused on patients with various types of atherosclerotic and vascular disease, whereas the alogliptin study targeted patients with recent acute coronary syndrome. Even with these differences, results of these two trials support the notion that DPP-4 inhibitors as a class do not lead to a significant increase or decrease in cardiovascular mortality. Key factors that may have impacted findings in these studies include the non-standardized use of other antihyperglycemics in both patient groups and relatively short follow up time (1.5-2.1 years), given the natural history of cardiovascular disease.
Other noteworthy studies this week:
In the Lancet Oncology, ten year follow up of breast cancer patients who received various doses and schedules of adjuvant radiation showed that hypofractionated regimens of 40 Gy were as effective as 50 Gy at preventing local and regional relapse [9].
In JAMA Internal Medicine, an observational study demonstrated that conjugated equine estrogens were associated with higher incidence of venous thrombosis than estradiol in postmenopausal women. Patients receiving conjugated equine estrogens also had laboratory evidence of propensity for clotting [10].
In JAMA, patients in Denmark who experienced cardiac arrest out of the hospital had better survival when bystanders performed CPR. This study was performed after the institution of several nationwide initiatives to increase CPR training to the general public, including making it a requirement for driver licensure [11].
In Science, subjects that read literary fiction immediately before cognitive and emotional testing performed better than those individuals who read popular fiction or non-fiction [12].
Dr. David Kudlowitz is a 1st year resident at NYU Langone Medical Center
Peer reviewed by Gregory Schrank, Internal Medicine, NYU Langone Medical Center
Image courtesy of Wikimedia Commons
References
1. Naci H and Ioannidis JPA. Comparative effectiveness of exercise and drug interventions on mortality outcomes: metaepidemiological study. BMJ. 2013;347:f5577. http://www.bmj.com/content/347/bmj.f5577
2. Fischer B, Jones W, Rehm J. High correlations between levels of consumption and mortality related to strong prescription opioid analgesics in British Columbia and Ontario, 2005-2009. Pharmacoepidimiol Drug Saf. 2013;22(4):438-442. http://onlinelibrary.wiley.com/doi/10.1002/pds.3404/abstract;jsessionid=B621FD500407427A3E634481B60479C6.f01t02
3. Dunn KM, Saunder KW, Rutter CM, et al. Opioid prescriptions for chronic pain and overdose. Ann Intern Med. 2010;152(2):85-92. http://annals.org.ezproxy.med.nyu.edu/article.aspx?articleid=745518
4. Raebel, MA, Newcomer SR, Reifler LM, et al. Chronic Use of Opioid Medications Before and After Bariatric Surgery. JAMA. 2013;310(3):1369-1376. http://jama.jamanetwork.com/article.aspx?articleid=1745677
5. Roumie CL, Hung AM, Greevy RA, et al. Comparative effectiveness of sulfonylurea and metformin monotherapy on cardiovascular events in type 2 diabetes mellitus: a cohort study. Annals of Internal Medicine. 2012;157(9):601-10. http://www.nejm.org/doi/full/10.1056/NEJMoa1307684
6. Lago RM, Sigh PP, Nesto RW. Congestive heart failure and cardiovascular death in patients with prediabetes and type 2 diabetes given thiazolidinediones: a meta-analysis of randomized clinical trials. Lancet. 2007;370:1129-36. http://www.nejm.org/doi/full/10.1056/NEJMoa1307684
7. Scirica BM, Bhatt DL, Braunwald E, et al. Saxagliptin and Cardiovascular Outcomes in Patients with Type 2 Diabetes Mellitus. NEJM. 2013;369:1317-26. http://www.nejm.org/doi/full/10.1056/NEJMoa1307684
8. White WB, Cannon CP, Heller SR, et al. Alogliptin after Acute Coronary Syndrome in Patients with Type 2 Diabetes. NEJM. 2013;369:1327-1335. http://www.nejm.org/doi/full/10.1056/NEJMoa1305889
9. Haviland JS, Owen JR, Dewar JA, et al. The UK Standardisation of Breast Radiotherapy (START) trials of radiotherapy hypofractionation for treatment of early breast cancer: 10-year follow-up results of two randomized controlled trials. The Lancet Oncology. 2013;14(11):1086-1094. http://www.thelancet.com/journals/lanonc/article/PIIS1470-2045%2813%2970386-3/fulltext
10. Smith NL, Blondon M, Wiggins KL, et al. Lower Risk of Cardiovascular Events in Postmenopausal Women Taking Oral Estradiol Compared With Oral Conjugated Equine Estrogens. JAMA Internal Medicine. 2013. Published online. http://archinte.jamanetwork.com/article.aspx?articleid=1741892
11. Wissenberg M, Lippert FK, Folke F, et al. Association of National Initiatives to Improve Cardiac Arrest management With Rates of Bystander Intervention and Patient Survival After Out-of-Hospital Cardiac Arrest. JAMA. 2013;310(13):1377-1384. http://jama.jamanetwork.com/article.aspx?articleid=1745678
12. Kidd DC, Castano E. Reading Literary Fiction Improves Theory of Mind. Science. Published Online Oct. 3, 2013. http://www.sciencemag.org.ezproxy.med.nyu.edu/content/early/2013/10/02/science.1239918.full