Peer Reviewed
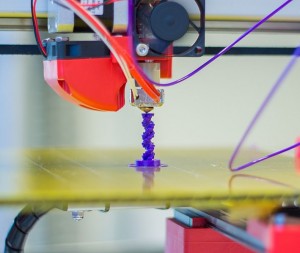
It seems that over the past week, New York has finally started to emerge from the deep-freeze of winter; and as we see the beginnings of spring, the lay press has begun to take interest in the eternal cycle of renewal. In particular, news has focused on the rapidly-expanding technology of 3D printing and the inroads it has been making into the science of organ growth [1]. When combined with these versatile devices, harvested and cloned cells can be used as a “bio-ink†to create complex structures that include vasculature, extracellular matrix, and multiple types of cells [2]. Success in this endeavor would be paradigm-changing for the field of transplant medicine, and could eventually topple the scarce-resource model upon which the organ sharing networks are based. In juxtaposition to the replacement of failing organs, this week’s edition of PrimeCuts looks at the opposite end of the medical spectrum with articles focused on screening for disease states, among other interesting developments.
Published in Thrombosis and Haemostasis, the SEARCH-AF study addresses the issue of screening for atrial fibrillation (AF) [3]. Commonly asymptomatic, AF can result in devastating morbidity and mortality through cardioembolic stroke – a risk that can be mitigated with systemic anticoagulation. In fact, although the American AF guidelines make no mention of screening [4], the European guidelines do recommend AF screening in adults over the age of 65 [5]. The SEARCH-AF trial, conducted in Australia was designed to determine the cost-effectiveness of a pharmacy-based community screening program for AF. With the use of an iPhone electrocardiogram application, screening was offered to 1,000 pharmacy customers over the age of 65. The investigators found 1.5% of screened adults to have newly discovered AF, all of whom had a CHA2DS2-VASc score greater than or equal to two. Based on existing AF data, including cost of screening and treatment, and expected benefits and risks of anticoagulation, a Monte Carlo simulation was performed showing the cost per quality adjusted life-year (QALY) gained to be $4,066 for this strategy of AF screening. Given that the cost-effectiveness threshold is generally set around $20,000 per QALY, this intriguing study suggests that community-based AF screening may be a useful tool in our preventative armamentarium. Important to note however, are the study’s limitations. Due to its small size, it is entirely plausible that the strategy used could have very different cost-effectiveness characteristics when applied in a different setting. Additionally, in any screening intervention, the ability to act on a positive result is paramount. As the study was conducted in Australia, a nation with universal healthcare, the pharmacists had easy access to the general practitioners caring for each person screened – a situation not completely echoed in our own healthcare system [6].
In another study focused on screening, a multitarget stool deoxyribonucleic acid (DNA) test was compared to fecal immunochemical testing (FIT) for the detection of colorectal cancer (CRC) [7]. The benefits of CRC screening have been well-established in terms of cancer-related mortality [8], but the fact remains that a sizable number of patients do not undergo screening, especially with the current gold-standard of colonoscopy [9]. This deficiency has fueled the search for an accurate, but less invasive, form of screening. In this study published in the New England Journal, results were analyzed for 9,989 patients at average risk for CRC who prospectively underwent stool DNA testing, FIT, and colonoscopy. In general, stool DNA testing was superior to FIT in terms of sensitivity (92.3% vs 73.8% for detecting CRC, p = 0.002; 42.4% vs 23.8% for detecting advanced precancerous lesions, p < 0.001) but inferior in terms of specificity (89.8% vs 96.4% in patients with negative colonoscopies, p < 0.001). When interpreting these results, however, it is important to remember that sensitivity is more pertinent than specificity in a screening test designed to exclude a serious disease state. Although the results of this study are also encouraging, it is difficult to consider the incorporation of stool DNA testing into a standard algorithm without the prospective validation of costs and testing intervals. Indeed, the United States Preventive Services Task Force currently recommends neither FIT nor stool DNA as a standard method of CRC screening [10].
With recent studies casting doubt on traditional approaches to mitigation of peri-operative cardiovascular risk, such as the use of beta-blockade [11], it should come as no surprise that the use of aspirin is also being re-examined. The POISE-2 investigators randomized 10,010 patients (stratified by baseline aspirin use) to aspirin or placebo prior to non-cardiac surgery with a primary composite endpoint of death or non-fatal myocardial infarction at 30 days [12]. Interestingly, there was no significant difference in this endpoint between the aspirin and placebo groups (7.0% vs 7.1%, hazard ratio [HR] 0.99, 95% confidence interval [CI] 0.86 to 1.15, p = 0.92), a finding which persisted on subgroup analysis, including baseline vs new aspirin use, pre-existing vascular disease, and Revised Cardiac Risk Index score. More intuitively, allocation to the aspirin arm did result in an increase in bleeding complications (HR 1.23, 95% CI 1.01 to 1.49, p = 0.04). Lest we begin to discontinue aspirin in all of our patients prior to surgery, a review of the study design reveals that any patient with a bare-metal stent within the past 6 weeks or a drug-eluting stent within the past year was excluded from participation, congruent with antithrombotic recommendations at the time the study was conducted [13]. That being said, the results of this trial do suggest that we consider a less aggressive stance on peri-operative continuation of aspirin when prescribed for less strong indications.
And finally, a study published in Circulation examines the safety of self-contained leadless cardiac pacemakers (LCP) [14]. The aptly named LEADLESS trial studied 33 patients undergoing placement of LCP with a primary endpoint of freedom from complications at 90 days. LCPs represent an effort to circumvent the complications of standard pacemakers (e.g. lead infection, lead fracture, lead dislodgment, pocket hematoma, and pocket infection) by avoiding both leads and pocket. The LCP itself is a small cylinder (42mm x 5.9mm) that is deployed through an endovascular approach and directly screwed into the right ventricular myocardium. In this non-randomized study, the complication-free rate was 94% – one patient suffered a right ventricular perforation and eventually died, and one patient had the LCP inadvertently implanted into the left ventricle necessitating removal and replacement. Although not the primary endpoint, the LCPs were all functioning as expected on three month followup. This study is limited by its small size and non-randomized design, and the LCPs themselves can only be used for right ventricular pacing without atrial sensing or pacing. However, the results of this trial still do pave the way for larger trials involving LCPs. If the technology proves to be safe and effective, pocket checks and laser lead extractions may become a thing of the past.
Other interesting reads this week:
Coming back to the topic of screening, an article in the British Medical Journal addresses the always-controversial question of prostate cancer [15]. This study suggests that a graded screening approach starting at age 60 may confer significant benefit in terms of cancer-related mortality.
An article in the Annals reviews the effectiveness of combination lipid-lowering therapy vs intensified statin monotherapy [16]. Although combination therapy appears to result in greater decreases in low-density lipoprotein as compared to statin monotherapy, clinical outcomes to support this strategy are lacking.
In JAMA, a study examines the efficacy of angiotensin converting enzyme inhibitors or angiotensin II receptor blockers in patients with advanced chronic kidney disease, hypertension, and anemia [17]. Even at advanced stages of disease (all patients had creatinine > 6 mg/dL), treatment decreases the risk of progression to dialysis without adversely impacting mortality.
In The Lancet Oncology, a study examines stereotactic radiosurgery as compared to whole-brain radiotherapy for patients with 5 to 10 brain metastases [18]. Radiosurgery was found to be non-inferior in terms of overall survival; the authors suggest it be considered for first line therapy given its better side-effect profile and minimally invasive nature.
Dr. Matthew Vorsanger is an associate editor, Clinical Correlations
Peer reviewed by Brian Greet, MD, associate editor, Clinical Correlations
Image Courtesy of Jonathan Juursema http://www.jonathanj.nl via Wikimedia Commons
References:
1. Griggs, Brandon. “The next frontier in 3-D printing: Human organs” cnn.com. CNN, 3 Apr. 2014.
2. Kolesky et al. 3D Bioprinting of Vascularized, Heterogeneous Cell-Laden Tissue Constructs. Adv Mater. 2014 Feb 18. Epub ahead of print. http://onlinelibrary.wiley.com/doi/10.1002/adma.201305506/abstract
3. Lowres et al. Feasibility and cost effectiveness of stroke prevention through community screening for atrial fibrillation using iPhone ECG in pharmacies. Thromb Haemost. 2014 Apr 1;111(6). Epub ahead of print. http://www.schattauer.de/en/magazine/subject-areas/journals-a-z/thrombosis-and-haemostasis/contents/archive/issue/special/manuscript/21004.html
4. Anderson et al. Management of patients with atrial fibrillation (compilation of 2006 ACCF/AHA/ESC and 2011 ACCF/AHA/HRS recommendations): A report of the American College of Cardiology/American Heart Association task force on practice guidelines. Circulation 2013; 127:1916-1926. http://www.sciencedirect.com/science/article/pii/S0735109713004956
5. Camm et al. 2012 focused update of the ESC Guidelines for the management of atrial fibrillation. An update of the 2010 ESC Guidelines for the management of atrial fibrillation. Developed with the special contribution of the European Heart Rhythm Association. Eur Heart J 2012; 33:2719-2747. http://europace.oxfordjournals.org/content/14/10/1385.long
6. The Australian Institute of Health and Welfare. http://www.aihw.gov.au/
7. Imperiale et al. Multitarget stool DNA testing for colorectal-cancer screening. N Engl J Med. 2014 Apr 3;370(14):1287-97. http://www.nejm.org/doi/full/10.1056/NEJMoa1311194
8. Shaukat et al. Long-term mortality after screening for colorectal cancer. N Engl J Med. 2013 Sep 19;369(12):1106-14. http://www.nejm.org/doi/full/10.1056/NEJMoa1300720
9. Vital signs: colorectal cancer screening test use — United States, 2012. MMWR Morb Mortal Wkly Rep 2013;62:881-8. http://www.cdc.gov/mmwr/preview/mmwrhtml/mm6244a4.htm
10. Screening for colorectal cancer: U.S. Preventive Services Task Force recommendation statement. Ann Intern Med 2008;149:627-37. http://annals.org/article.aspx?articleid=743535
11. Andersson et al. Association of β-Blocker Therapy With Risks of Adverse Cardiovascular Events and Deaths in Patients With Ischemic Heart Disease Undergoing Noncardiac Surgery: A Danish Nationwide Cohort Study. JAMA Intern Med. 2014 Mar 1;174(3):336-44. http://archinte.jamanetwork.com.ezproxy.med.nyu.edu/article.aspx?articleid=1779729
12. Devereaux et al. Aspirin in Patients Undergoing Noncardiac Surgery. N Engl J Med. 2014 Mar 31. Epub ahead of print. http://www.nejm.org/doi/full/10.1056/NEJMoa1401105
13. Douketis et al. The perioperative management of antithrombotic therapy: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines (8th Edition). Chest. 2008 Jun;133(6 Suppl):299S-339S. http://journal.publications.chestnet.org/article.aspx?articleid=1085932
14. Reddy et al. Permanent Leadless Cardiac Pacing: Results of the LEADLESS Trial. Circulation. 2014 Mar 24. Epub ahead of print. http://circ.ahajournals.org/content/early/2014/03/18/CIRCULATIONAHA.113.006987.long
15. Carlsson et al. Influence of blood prostate specific antigen levels at age 60 on benefits and harms of prostate cancer screening: population based cohort study. BMJ. 2014 Mar 28;348:g2296. http://www.bmj.com/content/348/bmj.g2296?view=long&pmid=24682399
16. Gudzune et al. Effectiveness of combination therapy with statin and another lipid-modifying agent compared with intensified statin monotherapy: a systematic review. Ann Intern Med. 2014 Apr 1;160(7):468-76. doi: 10.7326/M13-2526. http://annals.org/article.aspx?articleid=1828554
17. Hsu et al. Renoprotective effect of Renin-Angiotensin-aldosterone system blockade in patients with predialysis advanced chronic kidney disease, hypertension, and anemia. JAMA Intern Med. 2014 Mar 1;174(3):347-54. http://archinte.jamanetwork.com/article.aspx?articleid=1787693
18. Yamamoto et al. Stereotactic radiosurgery for patients with multiple brain metastases (JLGK0901): a multi-institutional prospective observational study. Lancet Oncol. 2014 Apr;15(4):387-95. http://www.thelancet.com/journals/lanonc/article/PIIS1470-2045(14)70061-0/fulltext