Peer Reviewed
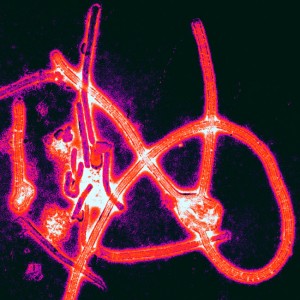
Infectious diseases remain at the forefront of news reports this week, as the largest Ebola outbreak on record continues. As of July 27th, the WHO reported greater than 1300 new cases and a devastating 729 deaths in Guinea, Liberia, and Sierra Leone since March of this year [1]. This past weekend saw the U.S. arrival of the first of two American aid workers who were infected with the virus while working in a hospital in Liberia [2]. This patient was transported to Emory University Hospital to receive treatment in an infectious disease containment unit, built under consultation from the nearby CDC. From this troubling news, we turn to a much more commonly encountered viral infection, with relatively robust treatment options, but still without a cure.
Can stem cell transplantation offer a prospective HIV cure?
While antiretroviral therapy (ART) can lead to undetectable HIV-1 RNA plasma levels, HIV reservoirs of latently infected cells, in which viral genome is integrated into host chromosomes, persist. Upon cessation of ART, a viral load rebound occurs with proliferation of these cells. One patient has famously achieved more than seven years of ART-free HIV-1 remission following myeloablative allogeneic hematopoietic stem cell transplantation (HSCT) for acute myeloid leukemia from a donor with a deletion in the gene encoding the HIV-1 coreceptor CCR5 [3]. In a recent article in Annals of Internal Medicine [4], the authors explore viral persistence in two previously reported patients with HIV and lymphoma, who likewise underwent HSCT, but with reduced-intensity condition and with CCR5 wild-type donor cells [5]. Both patients achieved full donor chimerism and recovery of CD4+ T cell counts following transplantation. Both also experienced significant clinical symptoms of graft-versus-host disease requiring immunosuppressive treatment. With continued suppressive ART, HIV-1 DNA was undetectable in peripheral blood mononuclear cells and no replication-competent HIV-1 was recovered from CD4+ T cells 4.3 years after HSCT in patient A and 2.6 years after HSCT in patient B.
The authors aimed to evaluate HIV reservoirs in these two patients through a closely monitored interruption of ART. They found detectable viremia 12 and 32 weeks after ART discontinuation in patients A and B, respectively. With HIV-naïve reconstituted immune systems, both patients also developed symptoms consistent with acute retroviral syndrome, and ART was re-initiated. The authors note that detectable viral levels usually rebound 1-8 weeks following ART interruption, hypothesizing that the delayed rebound viremia seen in these two patients was in part owing to an ongoing subclinical graft-versus-host reaction, with donor cell immune activity persistently clearing HIV-infected host cells. Sampling of the viremia revealed a high degree of genetic sequence homology, supporting the concept that HSCT with CCR5 wild-type donor cells potentiates a significant decrease in the HIV-1 reservoir, but that the small remnant viral burden is adequate for HIV-1 rebound following ART disruption. Though limited by a sample of only two patients, this study supports the need for further characterization of the HIV-1 reservoir.
Can non-antibiotic agents treat Clostridium difficile infections?
With C. diff infections increasing in frequency and severity, Johnson et al. studied the efficacy of three treatment options in two multinational double-blind randomized control trials [6]. As disruption of the native microbiome plays an important role in this infection, the authors aimed to compare the non-antimicrobial toxin-binding polymer tolevamer with metronidazole and vancomycin. A total of 1,118 adult patients with primary or recurrent toxin-confirmed, non-fulminant C. diff diarrheal infections were randomized in a 2:1:1 ratio to receive oral or nasogastric/jejunostomy tube-administered tolevamer for 14 days, metronidazole for 10 days, or vancomycin for 10 days (blinding maintained by dummy scheme of placebo administration to maintain uniform dosage timing). Clinical success was defined as resolution of diarrhea and severe abdominal discomfort for more than two consecutive days following treatment, while secondary endpoints included time to resolution of diarrhea and recurrence of C. diff infection. Ultimately, tolevamer proved inferior to both metronidazole and vancomycin in clinical success (44.2%, 72.7%, 81.1%, respectively, in combined analysis of the two trials; p < .001 for comparisons of tolevamer to metronidazole, and tolevamer to vancomycin). There was also longer time to resolution of diarrhea in the tolevamer group compared to the metronidazole and vancomycin groups. However, in patients who did respond to tolevamer, infection recurrence rates were notably decreased (4.5% tolevamer, 23.0% metronidazole, 20.6% vancomycin; p < .05 for comparisons of tolevamer to metronidazole, and tolevamer to vancomycin). While adverse event incidences were similar between the three treatment groups, a higher percentage of patients discontinued medication due to adverse events in the tolevamer group than in the metronidazole or vancomycin groups (25.5%, 11.2%, 6.5%, respectively; p < .01 for tolevamer vs metronidazole, p < .001 for tolevamer vs vancomycin). Interestingly, though a comparison of the two antibiotic treatments was not the intention, combined analysis of the two studies revealed greater clinical success with vancomycin treatment compared to metronidazole. While this study reaffirms the use of vancomycin for C. diff infections, recurrence rates following antibiotic treatment indicate that a toxin-binding alternative or therapeutic adjunct remains a worthwhile target for future investigation.
Should duration of routine cancer screening differ by health status?
Recommendations on when to cease routine cancer screening are guided by an evaluation of potential benefits (gained life-years, cancer-deaths prevented) weighed against potential harms (adverse events from screening, false-positives, overdiagnosis of cancers not likely to cause symptoms in an individual’s remaining lifetime). Current USPSTF recommendations direct breast cancer screening through age 74 [7] and colorectal cancer screening until age 75 [8], with consideration of individual health status. Intending to better define this individualization process for clinical utility, Lansdorp-Vogelaar and colleagues used simulation models to assess the impact of levels of comorbid conditions (none, mild, moderate, or severe) on the benefit versus harm analysis of breast, colorectal, and prostate cancer screening [9]. Mild comorbid conditions included history of MI, ulcer, or rheumatologic disease; moderate comorbidities included cardiovascular disease, paralysis, or diabetes; severe comorbid conditions included AIDS, COPD, liver disease, chronic renal failure, dementia, congestive heart failure, and combinations of conditions in the groups above. For each cancer site, they first generated a number needed to screen to gain one life-year (NNS/LYG) for persons age 74 with average health, and then compared these to NNS/LYG for individuals with the four levels of comorbid conditions. Pooling data from multiple simulation models, the authors found that in persons with no comorbid conditions, screening at the three sites could continue until a median age of 76 with similar harms/benefits to the “average-health†population aged 74. With mild comorbid conditions, the screening age with matched harms/benefits to the average person aged 74 was a median of 74 years; with moderate comorbid conditions, median of 72 years; with severe comorbid conditions, median of 66 years. The study has a number of limitations, most notably the unrealistic assumption that comorbid conditions impact life expectancy alone, and not cancer risk, progression, or survival. Nonetheless, the authors propose that these findings can aid in shaping cancer-screening discussions between providers and their individual elderly patients.
Are we forgetting to emphasize dietary modification to statin users?
With the ongoing obesity epidemic and increasing statin use in the past 25 years, the relationship between these anti-hyperlipidemics and a temporal trend in caloric and fat intake was examined in a cross-sectional study of 27,886 adults [10]. Using data collected from 1999 to 2010 in the National Health and Nutrition Examination Survey (NHANES), total reported caloric and fat intake were measured as primary outcomes, while secondary outcomes included serum levels of total cholesterol and LDL-C, as well as BMI. Compared to nonusers, statin users had more diagnoses of diabetes, a lower educational level, and were more likely to be older, male, and white. Adjusting for these sample differences, the author found that statin users consumed 179 kcal/d fewer calories (p = .007) and 9.5 g/d less fat (p = .003) than their nonusers counterparts in 1999-2000. Over the next decade, however, this difference between statin users and nonusers grew smaller, no longer showing statistical significance in 2003-2004 for fat intake and 2005-2006 for caloric intake. In 2009-2010, statin users actually consumed 54 kcal/d more calories and 2.7 g/d more fat than nonusers, although this gap lacked statistical significance. The authors further compared statin users with a stratified group of nonusers with hyperlipidemia, still finding a significant difference between the two (caloric intake p = .02, fat intake p = .01). Additionally, between the first and last examined time period, the study reports a BMI increase of 1.3 kg/m2 in statin users and only 0.4 kg/m2 in individuals not taking these agents (p = .02 for difference in trends). Predictably, the total cholesterol and LDL-C decreases during this period were greater in statin users than nonusers (p < .001 for both time trends). There are a few caveats in interpreting these results; among them is the survey’s reliance on a 24-hour dietary recall interview (allowing for numerous reporting biases) and the data’s representation of serial cross-sections rather than a cohort of the same individuals followed over time. Still, the authors posit that perhaps patients lost incentive to adhere to a modified diet upon seeing decreased LDL-C levels over time, and that physicians likewise may have moved from stressing diet management to emphasizing statin adherence.
ALSO IN THE JOURNALS THIS WEEK:
– An article in Science [11] delves into the molecular and cellular underpinnings of persistent HIV infection during antiretroviral treatment by examining three study participants’ HIV integration into cancer-associated genes to promote proliferation of virally infected cells during therapy.
– Since 2005, artemisinin-based combination therapies have been the WHO’s recommendation for first-line treatment of uncomplicated falciparum malaria in endemic countries [12], contributing to a significant decrease in international morbidity and mortality from malaria. This week, a report in The New England Journal of Medicine aimed to define the extent and severity of malarial resistance to artemisinin-based therapies that has emerged in western Cambodia and subsequently in areas of Southeast Asia [13]. Elsewhere in the issue, White and colleagues discuss a phase 2 trial to assess the efficacy, safety, and adverse-event profile of KAE609, a new synthetic antimalarial spiroindolone analogue with promising results against falciparum and vivax malaria [14].
– An article in Chest highlights the power of the mind (or rather its cortical functions) by reporting on the exacerbating impact of internally focused attention on idiopathic reflex cough, albeit with short-lived results [15]. Conversely, directing patients’ attention to external stimuli may offer therapeutic modulation of excessive cough.
Dr. Tamar Schiff is a 1st year resident at NYU Langone Medical Center
Peer reviewed by Karin Katz, MD, Internal Medicine Resident, NYU Langone Medical Center
Image courtesy of Wikimedia Commons
References
1. Ebola virus disease, West Africa – update. WHO. Retrieved from http://www.who.int/csr/don/2014_07_31_ebola/en/
2. Blinder, A., & Grady, D. (2014, August 2). American Doctor With Ebola Arrives in U.S. for Treatment. The New York Times. Retrieved from http://www.nytimes.com/2014/08/03/us/kent-brantley-nancy-writebol-ebola-treatment-atlanta.html?hp&action=click&pgtype=Homepage&version=HpSum&module=first-column-region®ion=top-news&WT.nav=top-news
3. Hütter G, Nowak D, Mossner M, Ganepola S, Müssig A, Allers K, et al. Long-term control of HIV by CCR5 Delta32/Delta32 stem-cell transplantation. N Engl J Med. 2009 Feb 12;360(7):692-8. doi: 10.1056/NEJMoa0802905. [http://www.nejm.org/doi/full/10.1056/NEJMoa0802905#t=article]
4. Henrich TJ, Hanhauser E, Marty FM, Sirignano MN, Keating S, Lee T, et al. Antiretroviral-Free HIV-1 Remission and Viral Rebound After Allogeneic Stem Cell Transplantation: Report of 2 Cases. Ann Intern Med. [Epub ahead of print 22 July 2014] doi:10.7326/M14-1027 [http://annals.org/article.aspx?articleid=1889547 ]
5. Heinrich TJ, Hu Z, Li JZ, Sciaranghella G, Busch MP, Keating SM, et al. Long-Term Reduction in Peripheral Blood HIV Type 1 Reservoirs Following Reduced-Intensity Conditioning Allogeneic Stem Cell Transplantation. J Infect Dis. (2013) 207 (11):1694-1702.doi: 10.1093/infdis/jit086 [http://jid.oxfordjournals.org/content/207/11/1694]
6. Johnson S, Louie TJ, Gerding DN, Cornely OA, Chasan-Taber S, Fitts D, et al. Vancomycin, Metronidazole, or Tolevamer for Clostridium difficile Infection: Results From Two Multinational, Randomized, Controlled Trials. Clin Infect Dis. 2014 Aug 1;59(3):345-54. doi: 10.1093/cid/ciu313. [http://cid.oxfordjournals.org/content/59/3/345.abstract]
7. U.S. Preventive Services Task Force. Screening for breast cancer: U.S. Preventive Services Task Force recommendation statement. Ann Intern Med. 2009 Nov 17;151(10):716-26, W-236. doi: 10.7326/0003-4819-151-10-200911170-00008
8. U.S. Preventive Services Task Force. Screening for colorectal cancer: U.S. Preventive Services Task Force recommendation statement. Ann Intern Med. 2008 Nov 4;149(9):627-37.
9. Lansdorp-Vogelaar I, Gulati R, Mariotto AB, Schechter CB, de Carvalho TM, Knudsen AB, et al. Personalizing Age of Cancer Screening Cessation Based on Comorbid Conditions: Model Estimates of Harms and Benefits. Ann Intern Med. 2014 Jul 15;161(2):104-12. doi: 10.7326/M13-2867 [http://annals.org/article.aspx?articleid=1887027]
10. Sugiyama T, Tsugawa Y, Tseng C, Kobayashi Y, Shapiro MF. Different Time Trends of Caloric and Fat Intake Between Statin Users and Nonusers Among US Adults: Gluttony in the Time of Statins?. JAMA Intern Med. 2014;174(7):1038-1045. doi:10.1001/jamainternmed.2014.1927. [http://archinte.jamanetwork.com/article.aspx?articleid=1861769]
11. Wagner TA, McLaughlin S, Garg K, Cheung CY, Larsen BB, Styrchak S., et al. Proliferation of cells with HIV integrated into cancer genes contributes to persistent infection. Science. 2014 Aug 1;345(6196):570-3. doi: 10.1126/science.1256304. [http://www.sciencemag.org/content/345/6196/570]
12. Overview of malaria treatment, WHO. Retrieved from http://www.who.int/malaria/areas/treatment/overview/en/
13. Ashley EA, Dhorda M, Fairhurst RM, Amaratunga C, Lim P, Suon S, et al. Spread of artemisinin resistance in Plasmodium falciparum malaria. N Engl J Med. 2014 Jul 31;371(5):411-23. doi: 10.1056/NEJMoa1314981. [http://www.nejm.org/doi/full/10.1056/NEJMoa1314981?query=featured_home]
14. White NJ, Pukrittayakamee S, Phyo AP, Rueangweerayut R, Nosten F, Jittamala P, et al. Spiroindolone KAE609 for falciparum and vivax malaria. N Engl J Med. 2014 Jul 31;371(5):403-10. doi: 10.1056/NEJMoa1315860. [http://www.nejm.org/doi/full/10.1056/NEJMoa1315860?query=featured_home]
15. Janssens T, Silva M, Davenport PW, Van Diest I, Dupont LJ, Van den Bergh O. Attentional Modulation of Reflex Cough. Chest. 2014;146(1):135-141. doi:10.1378/chest.13-2536. [http://journal.publications.chestnet.org/article.aspx?articleID=1832772]