 By Caroline Srisarajivakul, MD
By Caroline Srisarajivakul, MD
Peer Reviewed
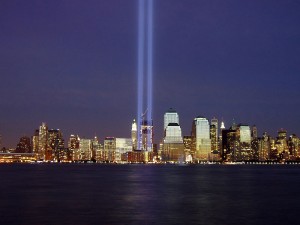
The invisible silhouettes of the Twin Towers loomed large in the minds of many New Yorkers last week as we marked the 13th anniversary of September 11th, 2001, while President Obama rallied the United States’ allies in the Middle East to unite against the Islamic State in Iraq and Syria prior to the terror group’s third videotaped beheading, this time of Briton David Haines. Meanwhile, in Western Africa, Ebola Virus Disease continues to ravage populations that are ill-equipped to handle this public health emergency, causing international health organizations to scramble to contain the largest recorded outbreak of this highly lethal, viral hemorrhagic fever.
PPI Use in Bleeding Ulcers – Is there a difference between intermittent use and continuous infusion?
In a 2012 guideline published on the management of ulcer-associated upper GI bleeding, the American College of Gastroenterology specifies a very particular regimen of proton-pump inhibitor (PPI) use: an 80mg IV bolus of a PPI followed by an 8mg/hr infusion for 72 hours in those patients who require endoscopic therapy for active bleeding or findings considered high-risk for rebleeding[1]. A new meta-analysis published in JAMA Internal Medicine[2] examined 13 randomized-controlled trials including 1691 patients comparing the standard bolus/infusion administration of a PPI in ulcer bleeds to intermittent bolus administrations of a PPI. The primary outcome examined was rebleeding rate at 7 days with several other secondary outcomes including rebleeding at 3 and 30 days, need for repeat endoscopic intervention, transfusion, length of hospitalization, need for surgery, and radiologic intervention. The analysis showed that the relative 7-day risk of rebleeding for intermittent vs continuous infusion was 0.72 (CI upper boundary of 0.97), and the absolute risk difference was -2.64%, which was below the pre-specified noninferiority margin of 3%, meaning that intermittent PPI boluses are not inferior to the standard bolus/infusion method of administering a PPI in upper ulcer-related GI bleeds. Furthermore, none of the secondary outcomes showed a statistically significant difference between the two regimens and all outcomes were below the noninferiority margin. Though there were flaws in the studies included in the meta-analysis, such as inconsistent blinding and allocation of patients, significant heterogeneity insofar as risk of bias was not found on subsequent subgroup analysis. The findings in this study suggest that in patients with ulcer-related upper GI bleeds that are treated endoscopically, continuous PPI infusion need not be a part of treatment, a finding that may help to resource utilization in the hospital setting.
Colchicine for Prevention of Postpericardiotomy Syndrome
This randomized controlled trial conducted at 11 centers in Italy examined the use of colchicine prior to and after cardiac surgery in reducing the rate of postpericardiotomy syndrome (PPS) in 360 patients[3]. PPS in this study was defined as having two of the following: fever without an alternative cause, pleuritic chest pain, friction rub, new or worsening pericardial effusion, or pleural effusion with an elevated CRP. Colchicine (0.5 mg twice daily in patients greater than or equal to 70 kg or 0.5 mg once daily in patients <70 kg) was given to the treatment group 1 or 2 days prior to surgery then continued for 1 month following the surgery with the primary outcome being incidence of PPS. The study found that 19.4% of patients in the colchicine group got PPS as compared to 29.4% in the placebo group (CI 1.1%-18.7%, NNT 10). There was no significant difference between the two groups insofar as the secondary outcomes of post-op atrial fibrillation or incidence of post-op pericardial and pleural effusions by intention-to-treat analysis. However,pre-specified subgroup analysis examining post-op atrial fibrillation in patients who completed the full course of treatment without discontinuing the drug due to side effects did show a significant difference between the two groups; 41.2% of patients in the placebo group developed post-op atrial fibrillation as opposed to 27% in the colchicine group (CI 3.3-24.7%, NNT=7). Drug discontinuation rates were similar in both groups (approx. 20%). This study demonstrated that colchicine has an important role in reducing morbidity from cardiac surgery, however, its well-known gastrointestinal adverse effects may limit its tolerability, raising the question of whether dose-reduction could help to mitigate these effects while still remaining effective in preventing PPS.
Withdrawing Inhaled Glucocorticoids in Patients with Severe COPD
In pulmonary news, a randomized controlled trial published in the New England Journal of Medicine examined the effect of withdrawing fluticasone therapy on subsequent moderate-to-severe COPD exacerbations in patients with severe COPD[4]. All 2485 patients in the study, who were predominantly white men, received either tiotropium or salmeterol as treatment for COPD and in the 6 weeks leading up to the study period, all patients received twice-daily fluticasone therapy. During the study period, control group patients continued to receive fluticasone. However, patients in the treatment group were tapered off of the fluticasone using dose reductions every 6 weeks with completion of the taper at 18 weeks. The study showed that the fluticasone taper was noninferior to continuation of therapy (HR 1.06, CI 0.94-1.19). There was also noninferiority in the study’s secondary outcomes, including time to first severe COPD exacerbation or rate of exacerbations. Analysis of spirometric parameters did show that in the fluticasone taper group, there was a statistically significant reduction in FEV1 (38mL) at week 18, a difference not present at weeks 6 or 12. This reduction in FEV1 did persist until the end of the follow period (42mL by the end of week 52). In the end, this study did show that, at least among white men, withdrawal of inhaled corticosteroid therapy did not have a significant effect on time to first moderate-to-severe exacerbation but did have a measurable effect on spirometric values such as FEV1. The clinical significance of this measured change in airflow is unclear.
Lung Cancer Screening in the Medicare Population
In 2011, the results of the National Lung Screening Trial (NLST) were published, showing that screening for lung cancer in high-risk patients ages 55-74 with annual low-dose CT scans (LDCT) reduced mortality as compared to screening with chest radiography[5]. Earlier this year the USPSTF issued a statement[6] recommending such screening up to the age of 80, though this has not been explicitly studied. Indeed, the original study included a population younger than those eligible for Medicare and this current secondary analysis[7] examined the NSLT data to clarify whether such a screening protocol would hold true in this older population. Patients in the NSLT were enrolled if they had a 30+ pack-year history and were current smokers or had quit within the past 15 years; they underwent annual LDCT for 3 years for the lung cancer screening. The secondary analysis showed that 7,110 patients over age 65 were more likely to have false-positives as compared with the cohort of 19,612 patients that were under 65 years old (27.7% vs. 22%) and also more likely to have invasive procedures as a result of the CT findings (3.3% vs 2.7%, which was statistically significant). There was no difference in complication rates from the invasive procedures done on false positives. The number needed to screen to prevent one lung cancer death in the older cohort was 245, and 364 in the younger cohort. In addition, the older population was more likely to have other clinically significant findings on the CT such as emphysema or cardiovascular abnormalities. Given the higher prevalence of lung cancer in older patients, the positive predictive value of a LDCT was, predictably, higher in the older cohort. This data demonstrates that LDCT screening in older patients has a mortality benefit at the trade-off of greater false positives and greater invasive procedures, which should make clinicians selective insofar as which patients should be offered screening.
Other notable publications this week:
The USPTF now recommends the use of low-dose aspirin prophylaxis in pregnant women at high risk for preeclampsia, an update to their 1996 guideline that found insufficient evidence to recommend for or against the use of aspirin for this indication.
An Australian study examining the consequences of cannabis use in adolescents has found a dose-dependent relationship between the amount of cannabis used and future use of other illicit drugs, cannabis dependence, and suicide attempts.
Patients who were previously on infliximab therapy for IBD and discontinued therapy due to drug reaction, loss of response, remission, or pregnancy can be safely retried on infliximab therapy.
Dr. Caroline Srisarajivakul is a second year resident at NYU Langone Medical Center
Peer reviewed by Mark H. Adelman, MD, Associate Editor, Clinical Correlations
Image courtesy of Wikimedia Commons
References:
1. Laine L, Jensen DM. Management of patients with ulcer bleeding. Am J Gastroenterol 2012; 107:345–360. http://gi.org/guideline/management-of-patients-with-ulcer-bleeding/
2. Sachar H, Vaidya K, Laine L. Intermittent vs Continuous Proton Pump Inhibitor Therapy for High-Risk Bleeding Ulcers: A Systematic Review and Meta-analysis. JAMA Intern Med. Published online 9/8/14. http://archinte.jamanetwork.com/article.aspx?articleid=1901116
3. Imazio M, Brucato A, Ferrazzi P, et al. Colchicine for Prevention of Postpericardiotomy Syndrome and Postoperative Atrial Fibrillation: The COPPS-2 Randomized Clinical Trial. JAMA 2014; 312(10):1016-1023. http://jama.jamanetwork.com/article.aspx?articleid=1900482
4. Magnussen H, Disse B, Rodriguez-Roisin R, et al. Withdrawal of Inhaled Glucocorticoids and Exacerbations of COPD. New Engl J Med. Published online 9/8/14. http://www.nejm.org/doi/full/10.1056/NEJMoa1407154
5. NLST Research Team. Reduced Lung-Cancer Mortality with Low-Dose Computed Tomographic Screening. N Engl J Med 2011; 365:395-409. http://www.nejm.org/doi/full/10.1056/NEJMoa1102873
6. Moyer VA. Screening for Lung Cancer: U.S. Preventive Services Task Force Recommendation Statement. Ann Intern Med. 2014; 160(5):330-338. http://annals.org/article.aspx?articleid=1809422
7. Pinsky PF, Gierada DS, Hocking W, et al. National Lung Screening Trial Findings by Age: Medicare-Eligible Versus Under-65 Population. Ann Intern Med. Published online 9/9/14. http://annals.org/article.aspx?articleid=1902271
8. LeFevre ML. Low-Dose Aspirin Use for the Prevention of Morbidity and Mortality From Preeclampsia: U.S. Preventive Services Task Force Recommendation Statement. Ann Intern Med. Published online 9/9/14. http://annals.org/article.aspx?articleid=1902275
9. Silins E, Horwood LJ, Patton GC, et al. Young adult sequelae of adolescent cannabis use: an integrative analysis. Lancet Psychiatry 2014; 1(4):286-293. http://www.thelancet.com/journals/lanpsy/article/PIIS2215-0366(14)70307-4/fulltext
10. Baert F, Drobne D, Gils A, et al. Early Trough Levels and Antibodies to Infliximab Predict Safety and Success of Reinitiation of Infliximab Therapy. Clin Gastroenterol Hepatol 2014; 12(9): 1474–1481.e2. http://www.cghjournal.org/article/S1542-3565(14)00141-4/abstract
