Vivian Hayashi MD, Robert Smith MD
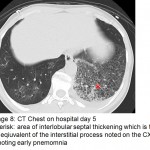
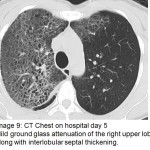
The answer to the mystery quiz is methicillin-resistant S. aureus (MRSA) pneumonia. The initial CXR (image 4) showed increased density in the area of the left hilum, hinting at a process in the superior segment of the left lower lobe. The next CXR (image 5) showed an airspace process in the left lower lobe that had rapidly evolved over 2 days. An interstitial process can be seen, as well, along with airspace disease (image 5, arrow). In addition, there is a suggestion of cavitation (image 5, asterisk). The third CXR (image 6) again shows rapid evolution of an infiltrate in the right upper lobe that also has a mixed interstitial-airspace appearance; the left lower lobe now has a more prominent area of consolidation (image 6, double asterisk). The chest CT (image 7) shows dense airspace consolidation of the left lower lobe including the superior segment, an air bronchogram and several areas of cavitation. Infiltration of the left superior segment was suspected from the initial CXR showing increased density over the left hilum. Chest CT (image 8, asterisk) shows the basilar area of the left lower lobe, not consolidated, but with interlobular septal thickening which is the CT equivalent of the interstitial change noted earlier on the CXR (image 5). Chest CT (image 9) again shows interlobular septal thickening with background ground glass attenuation of the right upper lobe. The rapidity of the evolving pneumonia allows us to view the different stages of the pneumonic process. Inflammation is first seen in the interstitium where engorged capillaries and interstitial edema give rise to radiographic interlobular septal thickening. The ground glass attenuation denotes early airspace infiltration by inflammatory fluid along with cellular infiltration. Lastly, the process evolves into dense consolidation of the airspace with, as in our case, necrosis or cavitation.
Community-acquired MRSA pneumonia is uncommon, but when identified, may be recognized by its aggressiveness, tendency for necrosis and cavitation (unlike pneumococcal or legionella pneumonia), and evidence of prior infection or colonization with the organism. In our case, we isolated MRSA from a routinely performed nasal swab which was the first hint of the causative pathogen. Subsequently, MRSA was isolated from a sputum culture. The organism also tested positive for the Panton-Valentine leukocidin (PVL) gene which is believed to mediate the destructiveness of the organism, evidenced in our case by the rapid course of the infection, cavitation and hemoptysis. The infection sometimes follows influenza infection; in our case, despite several days of myalgia and flu-like symptoms prior to hospitalization, testing for influenza A and B was negative. Although there is no convincing evidence that favors linezolid over vancomycin as therapy, we switched over to linezolid given our impression that the latter has better penetration into alveolar lining fluid and also better inhibition of PVL-related toxin synthesis.
Our patient recovered with remarkable clearing of the right upper lobe one week later (image 10). Appropriate antibiotics were started rather late in the hospital course (day 4), but fortunately, did abort the early ingress of infection in the right upper lobe.