Peer ReviewedÂ
“Indeterminate.” Many clinicians have expressed frustration when reading this word on a Quantiferon-TB Gold test result. The obligate follow-up question is: what is the next best step? Repeat the Quantiferon? Ignore it altogether and perform a Tuberculin Skin Test (TST) instead? Even worse, what happens when both tests are performed with discordant results? In order to answer some of these questions, this article begins with a very brief overview of Mycobacterium tuberculosis (TB) infection epidemiology. This is followed by a review of the tools currently available for the diagnosis of latent tuberculosis infection (LTBI). The last section explores some of the most important attributes of each test, which finally leads to a summary of a few of the current recommendations and the logic behind them.
A very brief overview of TB epidemiology and relevant definitions
Although it has been declared a global health emergency over 15 years ago by the World Health Organization (WHO), TB remains one of the leading infectious causes of morbidity in the world [5]. Every year, 8-10 million people globally develop active TB with an estimated 2 million annual deaths [2, 4, 5]. It is also estimated that one third of the world’s population (approximately 2 billion people) has LTBI [2, 6]. Definitions of LTBI vary slightly from organization to organization, but perhaps the most useful working definition is the one proposed by the World Health Organization (WHO): “a state of persistent immune response to prior-acquired Mycobacterium tuberculosis antigens without evidence of clinically manifested active TB” [18]. Persons with latent TB are classically considered to be not only asymptomatic but also noninfectious, and current evidence suggests that only 5-10% of people with LTBI develop active disease in their lifetime [1].
In the United States, the situation is slightly better than in other places in the world: the prevalence of active TB has declined from 6.2 cases per 100,000 people in 1998 to 4.2 cases per 100,000 in 2008. A TST survey in 2000 showed that approximately 11 million U.S. residents had LTBI, a 60% decline from 1972—although the decline was not uniform among all segments of the population and rates varied considerably [2, 7].
The currently available diagnostic tools
Despite the severity of this situation, the diagnostic tools for LTBI are not only few, but also have certain specific limitations. The most common tool in the arsenal of TB diagnosis is over 100 years old: the TST. It was not until 2001 that a new test became available, the QuantiFERON-TB test (QFT) (Cellestis Limited, Carnegie, Victoria, Australia). This was replaced in 2005 by its slightly more reliable descendant, the QuantiFERON-TB Gold test (QFT-G) (Cellestis Limited, Carnegie, Victoria, Australia), which in turn was replaced in 2007 by the most reliable version to date: the QuantiFERON-TB In-Tube test (QFT-IT) (Cellestis Limited, Carnegie, Victoria, Australia). Lastly, a separate tool that works on a similar mechanism as the Quantiferon tests became available in 2008: the T-SPOT.TB test (T-Spot) (Oxford Immunotec Limited, Abingdon, United Kingdom) [2].
In summary, three tools are currently in use for the diagnosis of LTBI, two of which fall under the same category:
- The time-honored Tuberculin Skin Test (TST)
- The Interferon-Gamma Release Assays (IGRAs), including:
- the QuantiFERON-TB In-Tube test (QFT-IT)
- the T-SPOT.TB test (T-Spot)
An Important Consideration
It is important to realize that both the TST and the IGRAs are useful for the diagnosis of latent TB, but have proven inadequate in the diagnosis of active TB. Three different systematic reviews/meta-analyses have consistently concluded that IGRAs can neither rule in nor rule out active TB (including extrapulmonary TB) [12, 13, 14]; the TST appears to have the same limitation.
The Tuberculin Skin TestÂ
The TST is the most commonly used tool worldwide for the diagnosis of LTBI. It consists of an intradermal injection of a poorly defined mixture of over 200 proteins derived from M. tuberculosis. A person with pre-existing cell-mediated immunity to these antigens will develop a delayed-type hypersensitivity reaction approximately 48-72 hours after the injection. This will cause swelling and induration at the site. A trained individual measures the lesion’s diameter, and the result is interpreted using pre-defined, risk-stratified cutoff points [1, 5, 6].
The Interferon-Gamma Release Assays
Just like the TST, the IGRAs (QFT-IT and T-Spot) measure a cell-mediated response. However, in the case of the IGRAs, a different aspect of the mechanism is analyzed. During infection, Th1 T-cells become sensitized to antigens naturally produced by M. tuberculosis and bind to them, releasing interferon-gamma (IFN-γ) in the process. The IGRAs work by using synthetic isolated antigens to induce a response in the existing T-cells of a patient’s whole blood sample. The T-cells bind to these antigens, their response is analyzed, and the results are interpreted by one of two protocols, depending on the specific IGRA:
QuantiFERON-TB In-Tube test
In the case of the QFT-IT, test antigens include early secretory antigenic target-6 (ESAT-6), culture filtrate protein 10 (CFP-10), and part of the peptide sequence for TB7.7. These antigens were specifically chosen because they are absent from BCG vaccine strains and most nontuberculous mycobacteria (with the exception of M. kansasii, M. szulgai, and M. marinum), thus increasing the QFT-IT’s specificity [2].
The test’s process is relatively simple: the antigens are incubated with the patient’s whole blood samples, and the amount of IFN-γ produced by T-cells is quantified via a single-step enzyme-linked immunosorbent assay (ELISA). The test relies on the basic principle that T-cells of an infected individual will release a significantly higher level of IFN-γ than those of a non-infected individual [3, 6].
In order to make the QFT-IT test more reliable, a total of three test tubes are provided for incubation (i.e. the test requires three blood samples): (1) the first one contains the test antigens, (2) the second one contains heparin alone (a negative control referred to as Nil), and (3) the third contains heparin, dextrose, and phytohemaglutinin (a positive control, referred to as the mitogen response). The results of the test are based on the amount of IFN-γ produced in each of the three test tubes, and the values of positive, negative, or indeterminate are defined based either on the manufacturer’s recommended criteria or on the criteria recommended by the specific country’s governing body (e.g. in the U.S., results are based on the criteria required by the FDA).
T-SPOT.TB test
Unlike the QFT-IT, the T-Spot’s antigens include only ESAT-6 and CFP-10. The test relies on the same basic principle as the QFT-IT, but instead of using ELISA to measure the amount of IFN-γ produced, the T-Spot uses an enzyme-linked immunospot assay (ELISPOT) on separated and counted peripheral blood mononuclear cells (PBMCs) to quantify the number of cells producing IFN-γ. The secreting cells appear as “spots” in each test well. The T-Spot also includes three tubes (requiring three blood samples): the test antigens, a negative control (Nil), and a positive control (mitogen response) [1, 2].
The results are based on the quantified number of spots (i.e. a representation of IFN-γ-secreting PBMCs) and, just like the QFT-IT, the values of positive, negative, or indeterminate are defined either by using the manufacturer’s recommendations or the criteria required by the specific country’s governing body [2].
The pros and cons of each test
TST
Some of the advantages of the TST are readily apparent. First, it is inexpensive—costs will vary from region to region, but as an example, the Los Angeles County Department of Public Health in California lists a per patient cost of $12.95 for a TST, compared to $21.27 for an IGRA [17]. The TST is also widely available and does not require complicated or expensive laboratory equipment. Furthermore, staff can be easily trained to measure the diameter of the induration and, based on the established protocols, come up with an interpretation of the test result (i.e. positive or negative).
The drawbacks, unfortunately, are significant. The first challenges are logistic: the test requires that the patient return to the clinic 2-3 days after administration of the injection, and the results are based on observation by trained staff, which introduces an element of subjectivity and therefore becomes a source of potential variability in interpretation [1]. Additionally, there are multiple factors that can affect TST interpretation—some of which may not always be reported by the patient or known beforehand by the clinician. Examples of these are those listed by the American Thoracic Society in conjunction with the Centers for Disease Control and Prevention [16], and include a history of gastrectomy or jejunoileal bypass, immigration from a high-prevalence country within five years of testing, silicosis, diabetes, certain types of cancer, recent weight loss of >10% ideal body weight, and many more. A relatively simplified list of the interpretation criteria for the TST is listed by the CDC at the following hyperlink [20]: http://www.cdc.gov/tb/publications/factsheets/testing/skintesting.htm.
Furthermore, there are two known potential sources for false positives: nontuberculous mycobacterium (NTM) infection and prior BCG vaccination [1, 6]. A study published in 2006 looked specifically at these two potential confounders [8], and their conclusions were as follows:
- If the BCG is received in infancy (i.e. within the first year of life), the effects on the TST are minimal—especially at greater than 10 years post-vaccination. Specifically, the study found that BCG vaccination in this group caused an overall rate of 8.5 false-positive TST reactions per 100 vaccines, with a rate of 2.6 false-positives per 100 vaccinations causing reactions of 15mm or more. When a TST was performed 10 years after vaccination, there was only one false positive per 100 vaccines.
- By contrast, BCG received after infancy or given multiple times (delivery of booster doses is common practice in some countries) produces more frequent, persistent, and larger TST responses. In this case, an overall rate of 41.8 false-positive TSTs (10mm or more) per 100 vaccines was observed. Of these, approximately half of the reactions were measured at greater than 15mm. Furthermore, this effect persisted when re-tested 10+ years after vaccination, albeit with a reduced rate of 21.2 false positives per 100 vaccines.
- NTM is not a clinically important cause of TST false positives, except in populations with a high prevalence of NTM sensitization and very low prevalence of TB infection, e.g., reasonably healthy adults in the Southern and Central U.S., certain parts of Sweden, and other industrialized countries.
Finally, false negatives may occur in particular patient subgroups, most importantly, the immunosuppressed—either due to medical conditions such as HIV infection, or iatrogenic immunosuppression, such as the immunosuppressive treatment of immune-mediated inflammatory diseases such as Crohn’s disease and rheumatoid arthritis [1, 5].
IGRAs (including QFT-IT and T-Spot)
The major advantage of IGRAs is their improved specificity in BCG-vaccinated patients, which is particularly important in countries where the BCG vaccine is administered after infancy or where booster shots are given [1, 6]. Logistically, the IGRAs only require one visit by the patient, result within 24 hours, and are free of the potential variability errors associated with TST placement and reading [2, 6].
A potential drawback of IGRAs is their significantly greater cost (including the need for specialized equipment) as compared to the TST; however, this cost may be offset by a decrease in false positives resulting in fewer resources spent evaluating and treating persons with positive test results [2, 5, 9]. Such a situation arises, for example, when testing BCG-vaccinated populations.
At least one study in the literature [6] argues that the main drawback of IGRAs is that their results “have not been validated prospectively, through follow-up of large cohorts, to determine the subsequent incidence of active TB.” This becomes particularly relevant in cases where an individual is IGRA-positive but TST-negative. This phenomenon remains unexplained, resulting in difficulties managing such patients.
When it comes to the immunosuppressed population, the available evidence suggests that IGRAs perform similarly to TST in detecting LTBI in HIV-infected individuals, and both TST and IGRAs have suboptimal sensitivity to detect active TB [1]. One could argue that the same limitations are likely to be present in the iatrogenically immunosuppressed population.
Finally, there is the question of whether a previous TST can affect IGRA results. The data are scarce at present, but a systematic review in 2009 concluded, “The TST appeared to affect IGRA responses only after 3 days and may apparently persist for several months” [10]. In other words, there is ongoing concern that a TST performed three or more days prior to an IGRA could lead to a false-positive IGRA.
Conclusions and pragmatic considerations when testing for LTBI
The information described above is but a glimpse into all of the current studies involving LTBI and its diagnostic challenges. In trying to summarize these into a pragmatic approach for the clinician, the following considerations seem reasonable:
Who to test
Both the TST and IGRAs may play a role in LTBI diagnosis. Use of these tests is appropriate among patients who are at risk for LTBI and would benefit from treatment (i.e. those at increased risk for developing active TB) [1, 2].
Who should NOT be tested
Generally, testing with TST and IGRAs should be avoided for persons at low risk for both latent infection and progression to active TB (unless they are likely to be at increased risk in the future) [2]. Additionally, as stated above, both tests have been shown to be inadequate for the diagnosis of active TB. If active TB is suspected, the clinician should proceed to acid-fast stain, culture, tissue pathology, imaging, bronchoscopy, etc. Consultation with an Infectious Diseases and/or Pulmonary specialist is warranted at this point.
Which test to use
Guidelines vary slightly from nation to nation—and within nations, from institution to institution. In general, the clinician should tailor the needs to the specific clinical scenario. That being said, given the overall characteristics of the available tests, some of the CDC’s 2010 recommendations state that “IGRA is preferred for testing persons from groups that historically have low rates of returning to have TSTs read” and “persons who have received BCG (as a vaccine or for cancer therapy).” On the other hand, “a TST is preferred for testing children aged <5 years” [2]. A full list of the CDC’s recommendations is beyond the scope of this article, but is available at the following website: http://www.cdc.gov/mmwr/preview/mmwrhtml/rr5905a1.htm.
If the choice of test hinges on BCG vaccination status and there is uncertainty regarding whether the patient has received the vaccine, the following BCG World Atlas [15] may prove useful to the clinician: http://www.bcgatlas.org/.
Should both tests be used sequentially? Simultaneously?
When a TST is read as borderline, the clinician may be tempted to draw an IGRA for confirmation. However, as mentioned above, there is ongoing concern about whether administration of a TST can produce a false-positive IGRA. The data are scarce at present and the question is still being studied, but in the interim, based on the findings of van Zyl-Smit et al’s systematic review [10], drawing an IGRA should be avoided if the patient has had a TST placed three or more days prior to the blood draw.
Regarding simultaneous use of both tests, a review of the literature revealed only one set of proposed guidelines for situations in which concurrent use of both tests is being considered: the Public Health Agency of Canada. Per its recommendation, if the clinician is to use both tests, in order to avoid problems with interpretation, blood samples for an IGRA should be drawn before or on the same day as placement of the TST [19].
Statistical validation of TST and IGRAs
The reader will have noticed that specific numbers for specificity, sensitivity, number needed to treat, and other statistical measures have not been listed. The reason for this is that assessments of such statistical measures (for both TST and IGRAs) vary widely depending on the source and, most importantly, are hampered by the basic fact that there is currently no gold standard to confirm a diagnosis of LTBI [2]. This is further complicated by the fact that test result interpretation criteria change from country to country, sometimes from organization to organization. Furthermore, determination of these values will change among different patient populations (e.g. infants, young children, HIV-positive patients, the immunocompromised, and so on). Sensitivity values for TST and IGRAs have been reported anywhere from ~60% to ~90% depending on the source, patient population, interpretation criteria, and so on.
That being said, in general, the IGRA’s sensitivity is estimated to be similar to that of the TST, but the specificity of IGRAs is generally considered to be higher—given that the antigens used in IGRAs are relatively specific to M. tuberculosis [2, 4]. There are discrepancies in the literature, but as an example, in persons unlikely to have M. tuberculosis infection, the CDC cites the QFT-IT’s specificity as 99%, compared to 85% for the TST [2]. Once again, these numbers will vary significantly based on the source, patient population, interpretation criteria, BCG status, and so on.
Thus, in summary, the choice of test should be based on the clinical scenario, institution-specific protocols, and expert recommendation (CDC, WHO, local Medical authorities).
A few additional considerations regarding result interpretation of both tests
Regarding the TST, when interpreting a positive value, it is important to consider more than just the size of the induration: the clinician should consider three different aspects: (1) the size of the induration, (2) the pretest probability of infection, and (3) the risk of disease if the person were truly infected [1].
Regarding IGRAs, “indeterminate” results are not uncommon with the QFT-IT—although this has improved when compared to its predecessors, the QFT and QFT-G. Indeterminate results are most often associated with age <5 years or >80 years, and with immunosuppression, e.g. from HIV infection or iatrogenic causes. In some instances, indeterminate results can be secondary to improper handling or insufficient samples (this is particularly true of the QFT and QFT-G, but also the QFT-IT). Per CDC recommendations, a repeat test can be useful when the initial IGRA was indeterminate and “a reason for testing persists,” or when assay measurements are unusual, e.g. when the mitogen response is lower than expected for the population being tested [2]. Otherwise, if available, a T-Spot may be more useful as it is associated with significantly fewer “indeterminate” results [2, 5]. If appropriate in such cases, a TST may also be considered. If doubt remains in spite of repeated, expanded testing, consultation with an Infectious Diseases specialist is warranted.
When to treat
A discussion regarding appropriate tests and treatment after the initial diagnosis of LTBI is beyond the scope of this article. However, a few items are worth mentioning: per the CDC’s recommendations, the diagnosis and treatment of M. tuberculosis infection should NOT be based on IGRA or TST results alone. Other considerations need to be included in the decision, such as epidemiologic and medical history, risk factors and overall clinical picture [2]. A useful tool for the clinician is the Online TST/IGRA Interpreter [11] at http://www.tstin3d.com/. This website helps the clinician estimate the risk of progression to active TB for an individual who has undergone TST or IGRA testing given the specific clinical picture, including items such as country of birth, age at immigration to a country with low TB incidence, existing comorbidities, and many more.
Mycobacterium tuberculosis infection is a complex, even elegant process with significant individual and public health implications. Clearly further research is needed in the field of diagnostics. In the meantime, it is the writer’s hope that this article sheds some light on the advantages and limitations of the currently available tests for latent disease, which will hopefully in turn assist the clinician in making a better-informed test choice.
Dr. Miguel A. Saldivar, MD is a 3rd year resident at NYU Langone Medical Center
Peer reviewed by Howard Leaf, MD, Internal Medicine, NYU Langone Medical Center
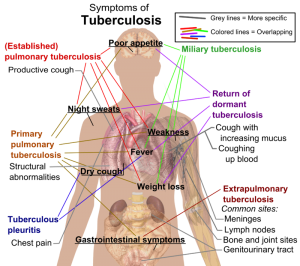
Image courtesy of Wikimedia CommonsÂ
References
- Pai M, Denkinger CM, Kik SV, et al. Gamma interferon release assays for detection of Mycobacterium tuberculosis infection. Clin Microbiol Rev. 2014 Jan;27(1):3-20. doi: 10.1128/CMR.00034-13. PMID 24396134. http://cmr.asm.org/content/27/1/3.long
- Mazurek GH, Jereb J, Vernon A, et al. Updated guidelines for using Interferon Gamma Release Assays to detect Mycobacterium tuberculosis infection – United States, 2010. MMWR Recomm Rep. 2010 Jun 25;59(RR-5):1-25. PMID 20577159. http://www.cdc.gov/mmwr/preview/mmwrhtml/rr5905a1.htm
- Smith DS. Interferon Gamma Release Assays. Stanford University. http://web.stanford.edu/group/parasites/ParaSites2006/TB_Diagnosis/Interferon%20Gamma%20Release%20Assays.html
- Lalvani A. Diagnosing tuberculosis infection in the 21st century: new tools to tackle an old enemy. Chest. 2007 Jun;131(6):1898-906. PMID 17565023. http://journal.publications.chestnet.org/article.aspx?articleid=1085168
- Lalvani A, Pareek M. Interferon gamma release assays: principles and practice. Enferm Infecc Microbiol Clin. 2010 Apr;28(4):245-52. doi: 10.1016/j.eimc.2009.05.012. Epub 2009 Sep 24. PMID 19783328. http://www.elsevier.es/en-revista-enfermedades-infecciosas-microbiologia-clinica-28-articulo-interferon-gamma-release-assays-principles-13149868
- Landry J, Menzies D. Preventive chemotherapy. Where has it got us? Where to go next? Int J Tuberc Lung Dis. 2008 Dec;12(12):1352-64. PMID 19017442. http://www.ingentaconnect.com/content/iuatld/ijtld/2008/00000012/00000012/art00005?token=0051132cf33437a63736a6f3547414c7d703444532e5b6f644a467b4d616d3f4e4b3485763504194f
- Bennett DE, Courval JM, Onorato I, et al. Prevalence of tuberculosis infection in the United States population: the national health and nutrition examination survey, 1999–2000. Am J Respir Crit Care Med. 2008 Feb 1;177(3):348-55. Epub 2007 Nov 7. PMID 17989346. http://www.atsjournals.org/doi/abs/10.1164/rccm.200701-057OC?url_ver=Z39.88-2003&rfr_id=ori:rid:crossref.org&rfr_dat=cr_pub%3dpubmed#.VOpDnnaR_RI
- Farhat M, Greenaway C, Pai M, Menzies D. 2006. False-positive tuberculin skin tests: what is the absolute effect of BCG and nontuberculous mycobacteria? Int. J. Tuberc. Lung Dis. 10:1192–1204. PMID 17131776. http://www.ingentaconnect.com/content/iuatld/ijtld/2006/00000010/00000011/art00003?token=00561c5878e77900a6855c5f3b3b47465248703b444549794624734f582a2f4876753375686f49530b0a5c
- Marra F, Marra CA, Sadatsafavi M, et al. Cost-effectiveness of a new interferon-based blood assay, QuantiFERON-TB Gold, in screening tuberculosis contacts. Int J Tuberc Lung Dis. 2008 Dec;12(12):1414-24. PMID 19017451. http://www.ingentaconnect.com/content/iuatld/ijtld/2008/00000012/00000012/art00014?token=00501d71712f1753f11c939412f415d766b2544453a4a6c7b73516f253048296a7c2849266d656cc
- van Zyl-Smit RN, Zwerling A, Dheda K, Pai M. Within-subject variability of interferon-g assay results for tuberculosis and boosting effect of tuberculin skin testing: a systematic review. PLoS One. 2009 Dec 30;4(12):e8517. doi: 10.1371/journal.pone.0008517. PMID 20041113. http://journals.plos.org/plosone/article?id=10.1371/journal.pone.0008517
- Law S, Menzies D, Pai M, et al. The Online TST/IGRA Interpreter. McGill University & McGill University Health Center, Montreal Quebec. Canada. http://www.tstin3d.com/
- Metcalfe JZ, Everett CK, Steingart KR, et al. Interferon-γ release assays for active pulmonary tuberculosis diagnosis in adults in low- and middle-income countries: systematic review and meta-analysis. J Infect Dis. 2011 Nov 15;204 Suppl 4:S1120-9. doi: 10.1093/infdis/jir410. 21996694. http://jid.oxfordjournals.org/content/204/suppl_4/S1120.full?sid=1dad36e7-34b2-4950-a694-108659642e9b
- Sester M, Sotgiu G, Lange C, et al. Interferon-γ release assays for the diagnosis of active tuberculosis: a systematic review and meta-analysis. Eur Respir J. 2011 Jan;37(1):100-11. doi: 10.1183/09031936.00114810. Epub 2010 Sep 16. PMID 20847080. http://erj.ersjournals.com/content/37/1/100.long
- Fan L, Chen Z, Hao XH, et al. Interferon-gamma release assays for the diagnosis of extrapulmonary tuberculosis: a systematic review and meta-analysis. FEMS Immunol Med Microbiol. 2012 Aug;65(3):456-66. doi: 10.1111/j.1574-695X.2012.00972.x. Epub 2012 Jun 18. PMID 22487051. http://femsim.oxfordjournals.org/content/65/3/456
- Zwerling A, Behr M, Verma A, et al. The BCG World Atlas. A Database of Global BCG Vaccination Policies and Practices. McGill University & McGill University Health Center, Montreal Quebec. Canada. PLoS Med. 8:e1001012. http://dx.doi.org/10.1371/journal.pmed.1001012. http://www.bcgatlas.org.
- Targeted Tuberculin Testing and Treatment of Latent Tuberculosis Infection. American Journal of Respiratory and Critical Care Medicine, Vol. 161 (2000). Supplement: American Thoracic Society/Centers for Disease Control and Prevention-Targeted Tuberculin Testing and Treatment of Latent Tuberculosis Infection (2000), pp. S221-S247. doi: 10.1164/ajrccm.161.supplement_3.ats600. http://www.atsjournals.org/doi/full/10.1164/ajrccm.161.supplement_3.ats600#.VOoQsnaR_RI
- Direct Costs of TST/IGRA Cost Effectiveness. Los Angeles Department of Public Health, Division of HIV and STD Programs. State of California. http://publichealth.lacounty.gov/dhsp/MAC/IGRAcosteffectiveness.pdf
- World Health Organization (WHO). Guidelines on the Management of Latent Tuberculosis Infection. ISBN: 978 92 4 154890 8. WHO reference number: WHO/HTM/TB/2015.01. http://www.who.int/tb/publications/ltbi_document_page/en/
- Updated Recommendations on Interferon Gamma Release Assays for Latent Tuberculosis Infection. An Advisory Committee Statement of the Canadian Tuberculosis Committee. Volume 34, ACS-6, October 2008. http://www.phac-aspc.gc.ca/publicat/ccdr-rmtc/08vol34/acs-6/index-eng.php.
20. Fact Sheets: Tuberculin Skin Testing. Cetners for Disease Control and Prevention. http://www.cdc.gov/tb/publications/factsh