Peer Reviewed
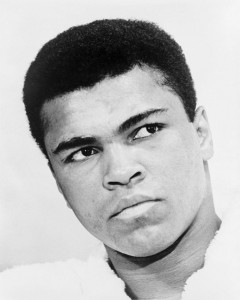
This week boxing champion and international legend Muhammad Ali passed away at the age of 74. Ali has been recognized as one the best, if not the best, heavyweight boxer the sport has ever seen [1]. But it wasn’t just his athletic prowess that distinguished him; Ali was known for his religious views, his strong political stances, and his very publicized battle with Parkinson’s disease. Barack and Michelle Obama summed it up nicely when they remarked on “how fortunate we are that The Greatest chose to grace our time” [2].
Speaking of great athletes of our time, Novak Djokovic beat out Andy Murray to finally clinch the French Open title [3]. With this win, Djokovic became the eighth man in history to complete the career Grand Slam. Additionally, with this win, Djokovic is in line to potentially achieve a true Grand Slam by winning all four Grand Slam tournaments in the same year.
As we continue to celebrate great athletes, past and present, we turn to celebrate and acknowledge the most recent advances in medical literature this week.
Long Term Follow Up of Fecal Microbiota Transplantation for Severe and/or Complicated Clostridium difficile Infection
Fecal microbiota transplantation (FMT) refers to the practice of taking stool from a healthy individual and introducing it into the gut of a sick individual to cure a specific disease. This treatment method has gained increased favor in treating patients with Clostridium difficile infection (CDI), and in 2013 the American College of Gastroenterology guidelines for managing CDI recommended FMT as an alternative treatment for patients after three or more CDI recurrences [4]. The efficacy of FMT in severe and/or complicated CDI, however, has yet to be investigated.
A multicenter long-term follow-up study published in the Journal of Clinical Gastroenterology looked at the response to FMT for 17 individuals with severe and/or complicated CDI[5]. Severe CDI was defined as the presence of significant abdominal tenderness, albumin <3g/dL or white count >15,000 cells/μL. Complicated CDI was defined as the presence of at least one of the following criteria that could be attributed to CDI: admission to the ICU, hypotension with or without the use of vasopressors, fever, ileus, severe abdominal tenderness, change in mental status, white count >35,000 cells/μL or <2000 cells/μL, serum lactate >2.2mmol/L, and end-organ failure. In terms of symptoms, diarrhea improved in 25% after FMT and resolved entirely in 75% after FMT with mean time to resolution of symptoms 5.7 days. Abdominal pain resolved in 72.7% and improved in 27.3% after FMT. Primary cure without early CDI recurrence (< 90d) after FMT was seen in 88.2% of patients. Secondary cure rate (cure after a second FMT) was 94.1%. Patients tolerated the FMT well without any direct adverse events. Overall, FMT appears to be a safe and effective therapy for patients with severe and/or complicated CDI, however, given the relatively small sample size of this study, more data is needed prior to recommending the use of FMT as standard therapy for this cohort of patients.
Comparable Outcomes for Critically Ill Patients Cared for by Acute Care Nurse Practitioners and Resident Teams
In many intensive care units throughout the country, acute care nurse practitioners (ACNPs) and physician assistants (PAs) have been employed in recent years to assist in staffing units that have limited manpower given resident duty hour restrictions. Additionally the number of intensivists is insufficient to meet the increasing demand in critical care units. A recent prospective cohort study sought to investigate long-term outcomes for critically ill patients continually cared for by ACNPs [6].
In this study, there were 9066 admissions to an ICU service with 2366 cared for by ACNPs and 6700 cared for by a resident team. A primary endpoint of 90-day survival was used to compare ACNP teams to resident teams. A multivariate analysis was conducted and there was no difference found between the ACNP and resident teams in the primary outcome. Patients admitted to the ACNP service had lower ICU mortality than resident team patients (6.3% versus 11.6%, P = 0.01) however hospital mortality showed no statistical difference.
This study differed from others evaluating advanced care providers in the critical care setting in various ways. The ACNPs cared for patients continuously throughout their ICU stay without fellows or attendings covering at night. Additionally, this study followed up with patients beyond hospital discharge, further strengthening the evidence that ACNP care is comparable to resident care during hospitalization as well as after discharge.
Early Initiation of Renal Replacement Therapy May Reduce Mortality in Critically Ill Patients with Acute Kidney Injury
Acute kidney injury (AKI) is a commonly seen entity in critically ill patients. There have been many advances in the management of AKI, especially in those with life-threatening complications, however it has remained unclear what the best management strategy is for those with AKI who do not yet have those complications. A randomized single-center clinical trial was published in JAMA this past week evaluating the optimal timing of initiating renal replacement therapy (RRT) in those with severe AKI without life-threatening indications. [7].
231 critically ill patients with AKI Kidney Disease: Improving Global Outcomes (KDIGO) stage 2 and plasma neutrophil gelatinase-associated lipocalin level higher than 150ng/mL were enrolled in the study. The patients were randomly assigned to either undergo early RRT (within 8 hours of diagnosis of KDIGO stage 2) or delayed RRT (within 12 hours of stage 3 AKI or no initiation). The primary endpoint was 90-day mortality after randomization with various secondary endpoints including 28- and 60-day mortality, evidence of organ dysfunction, recovery of renal function, duration and need for persistent renal support, and ICU and hospital length of stay. Early initiation of RRT was shown to significantly reduce 90-day mortality compared with delayed initiation of RRT (39.3% versus 54.7% mortality, P=0.03). The early initiation group also had better renal recovery by day 90 (53.6% versus 38.7%, P=0.02) and shorter RRT duration and length of hospital stay (RRT: 9 days in the early group versus 25 days in the delayed group; P = .04; hospital stay: 51 days in the early group versus 82 days in the delayed group; P < .001). There was no significant difference in need for RRT after day 90, organ dysfunction, or length of ICU stay. Although more data is needed on this topic, this study provides compelling evidence for the early initiation of RRT in critically ill patients with non-life threatening AKI.
Routine Pre-Procedural Administration of Rectal Indomethacin Reduces Overall Occurrence of Post-ERCP Pancreatitis
Acute pancreatitis is the most common complication of endoscopic retrograde cholangiopancreatography (ERCP), and the use of rectal NSAIDs in high-risk populations has been shown to decrease the incidence of this complication. A multicenter, single-blinded, randomized controlled trial out of China sought to investigate whether routine pre-procedural administration of rectal indomethacin versus selective post-procedural rectal indomethacin decreases the overall occurrence of post-ERCP pancreatitis [8]. 2600 patients were randomized to universal pre-procedure indomethacin or post-procedural indomethacin in high-risk patients. The primary outcome was overall occurrence of post-ERCP pancreatitis. Post-ERCP pancreatitis occurred in 6% of high-risk patients in the universal group and 12% of high-risk patients in the risk-stratified group (P=0.0057). Post-ERCP pancreatitis was less frequent in average-risk patients in the universal group (3%) than in the risk-stratified group (6%) where they did not receive the drug (P=0.0003). The practice of administering routine pre-procedure rectal indomethacin prior to ERCP decreased the overall occurrence of post-ERCP pancreatitis without an increase in adverse effects.
Mini cuts:
A randomized clinical trial of patients with emphysema and severe air trapping looked at the effect of usual care (bronchodilators, pulmonary rehabilitation) versus usual care plus bilateral endobronchial coil treatment on exercise tolerance [9]. Although there was a slight improvement in exercise tolerance in those patients who received endobronchial coils, the incidence of major complications was also greater. More studies are needed to determine the utility of this treatment method.
Treatment with an aromatase inhibitor for 5 years has been the standard of therapy for hormone-receptor-positive early breast cancer in postmenopausal women, however a new study looked at extending treatment to 10 years [10]. This change in treatment duration was associated with increased rates of disease-free survival and lower incidence of contralateral breast cancer.
Particulate air pollution and traffic-related air pollutants are associated with cardiovascular risk. A prospective 10-year cohort study published in the Lancet sought to determine the underlying disease process contributing to this association [11]. The study demonstrated that increased concentrations of particulate air pollution and traffic-related air pollutants are associated with progression in coronary calcification, and therefore may be contributing to accelerated atherosclerosis.
Dr. Dana Zalkin is a 1st-year resident at NYU Langone Medical Center.
Peer reviewed by Dr. Amar Parikh, 2nd year internal medicine resident at NYU Langone Medical Center
Image courtesy of Wikimedia Commons
References:
[1] Lipsyte, Robert. “Muhammad Ali Dies at 74: Titan of Boxing and the 20th Century.” The New York Times. The New York Times, 03 June 2016. Web. 05 June 2016.
[2] “President Obama’s Statement on Muhammad Ali.” The New York Times. The New York Times, 04 June 2016. Web. 05 June 2016.
[3] Clarey, Christopher. “Novak Djokovic Beats Andy Murray to Claim Elusive French Open Title.” The New York Times. The New York Times, 05 June 2016. Web. 05 June 2016.
[4] Surawicz CM, Brandt LJ, Binion DG, et al. Guidelines for diagnosis, treatment, and prevention of Clostridium difficile infections. Am J Gastroenterol. 2013;108:478–498.
[5] Aroniadis OC, Brandt LJ, Greenberg A, Borody T, Kelly CR, Mellow M, Surawicz C, Cagle L, Neshatian L, Stollman N, Giovanelli A, Ray A, Smith R. Long-term Follow-up Study of Fecal Microbiota Transplantation for Severe and/or Complicated Clostridium difficile Infection: A Multicenter Experience. J Clin Gastroenterol. 2016 May-Jun;50(5):398-402. doi: 10.1097/MCG.0000000000000374. PubMed PMID: 26125460. http://journals.lww.com/jcge/Abstract/2016/05000/Long_term_Follow_up_Study_of_Fecal_Microbiota.11.aspx
[6] Landsperger JS, Semler MW, Wang L, Byrne DW, Wheeler AP. Outcomes of Nurse Practitioner-Delivered Critical Care: A Prospective Cohort Study. Chest. 2016 May;149(5):1146-54. doi: 10.1016/j.chest.2015.12.015. Epub 2015 Dec 28. PubMed PMID: 26836900. http://www.ncbi.nlm.nih.gov/pubmed/26836900
[7] Zarbock A, Kellum JA, Schmidt C, et al. Effect of Early vs Delayed Initiation of Renal Replacement Therapy on Mortality in Critically Ill Patients With Acute Kidney Injury: The ELAIN Randomized Clinical Trial. JAMA. 2016;315(20):2190-2199. doi:10.1001/jama.2016.5828. http://jama.jamanetwork.com/article.aspx?articleid=2522434
[8] Luo H, Zhao L, Leung J, et al. Routine pre-procedural rectal indomethacin versus selective post-procedural rectal indomethacin to prevent pancreatitis in patients undergoind ERCP: a multicenter, randomized controlled trial. Lancet. 2016:387(10035): 2293-2301. http://www.download.thelancet.com/journals/lancet/article/PIIS0140-6736(16)30310-5/fulltext
[9] Sciurba FC, Criner GJ, Strange C, et al. Effect of Endobronchial Coils vs Usual Care on Exercise Tolerance in Patients With Severe Emphysema: The RENEW Randomized Clinical Trial. JAMA. 2016;315(20):2178-2189. doi:10.1001/jama.2016.6261. http://jama.jamanetwork.com/article.aspx?articleid=2522517
[10] Goss, Paul E., James N. Ingle, Kathleen I. Pritchard, Nicholas J. Robert, Hyman Muss, Julie Gralow, Karen Gelmon, Tim Whelan, Kathrin Strasser-Weippl, Sheldon Rubin, Keren Sturtz, Antonio C. Wolff, Eric Winer, Clifford Hudis, Alison Stopeck, J. Thaddeus Beck, Judith S. Kaur, Kate Whelan, Dongsheng Tu, and Wendy R. Parulekar. “Extending Aromatase-Inhibitor Adjuvant Therapy to 10 Years.” New England Journal of Medicine N Engl J Med (2016). Web. 5 June 2016. http://www.nejm.org/doi/full/10.1056/NEJMoa1604700?query=featured_home
[11] Kaufman JD, Adar SD, Barr RG, Budoff M, Burke GL, Curl CL, Daviglus ML, Roux AV, Gassett AJ, Jacobs DR Jr, Kronmal R, Larson TV, Navas-Acien A, Olives C, Sampson PD, Sheppard L, Siscovick DS, Stein JH, Szpiro AA, Watson KE. Association between air pollution and coronary artery calcification within six metropolitan areas in the USA (the Multi-Ethnic Study of Atherosclerosis and Air Pollution): a longitudinal cohort study. Lancet. 2016 May 24. http://www.thelancet.com/journals/lancet/article/PIIS0140-6736(16)00378-0/abstract