Peer Reviewed
Welcome to Gamechangers, a series that takes a critical look at the latest in medical literature to answer one important question: would the results of this article change my practice? Featuring thorough evidence-based review as well as expert commentary, our aim is for this series to help you decide if the results of a given study are, in fact, a gamechanger.Â
Why does this matter?
Community-acquired pneumonia (CAP) is a common and potentially serious infection that can lead to hospitalization and death.[1,2]  While antibiotics have been the mainstay for treatment of CAP, systemic steroids have been postulated to augment antibiotics in the treatment of pneumonia since as early as the 1950s.[3] Multiple systematic reviews and meta-analyses about the use of steroids in severe CAP have been published in the last decade.[4,5,6], Most of these analyses demonstrate that steroids decrease length of hospitalization for CAP and some suggest steroids decrease mortality, especially in severe CAP. Until recently, the body of research for use of adjunctive steroids in moderate CAP was limited to two small studies with discordant results.[7,8] Furthermore, the study that demonstrated efficacy of steroids in CAP has limited generalizability due to the use of intravenous dexamethasone. In April 2015 the results of the STEP (“Corticosteroid treatment for community-acquired pneumoniaâ€) trial was published which randomized nearly 800 patients with CAP of varying severity to adjunctive oral prednisone vs placebo.[9]
How was the study designed?
The STEP study was a multicenter, double-blind, randomized, placebo-controlled trial that took place in seven tertiary care hospitals in Switzerland from Dec 2009 to May 2014. Patients were eligible for enrollment if they met the following criteria: age 18 years or older and admitted to the hospital with CAP, which was defined as an infiltrate on chest radiograph plus one other sign or symptom of pneumonia (e.g. cough, sputum production, fever, leukocytosis, etc.). Exclusion criteria included permanent inability to give informed consent as well as reasons to avoid steroids such as recent GI bleed, immunosuppression and pregnancy, or reasons to withhold steroids in the placebo group such as known adrenal insufficiency or ongoing corticosteroid use.
Eligible patients were designated to receive either 50mg oral prednisone or placebo daily for 7 days through centralized randomization lists and prepackaged medications to ensure appropriate randomization and blinding. Baseline blood samples were drawn and patients were started on European guideline-based antibiotic therapy, which included either amoxicillin-clavulanic acid or ceftriaxone monotherapy. Clarithromycin was added for those patients with atypical organisms or requiring ICU care.  A procalcitonin-guided therapy algorithm was encouraged, but clinical decisions and discharge time was at the discretion of the treating team.
The primary outcome of the STEP trial was time to clinical stability defined as stable vital signs with baseline mental status and ability to tolerate oral nutrition for 24 hours. Secondary endpoints included time to discharge, pneumonia recurrence, re-admission, ICU admission, all-cause mortality, duration of total and IV antibiotic treatment, validated disease activity scores specific to CAP and complications of CAP (acute respiratory distress syndrome (ARDS), empyema, respiratory failure, etc.). Investigators also evaluated adverse effects of glucocorticoids including rate of hyperglycemia, hypertension, delirium, nosocomial infections and weight gain.
What were the study results?
Of the 1,407 patients who met inclusion criteria, 785 ended up in final intention-to-treat groups: 392 in the prednisone group and 393 in the placebo group. Patients in this study tended to be older, with a median age of 74 years, and had high burden of comorbid chronic illnesses including diabetes (20%), chronic obstructive pulmonary disease (COPD) (17%), congestive heart failure (18%) and chronic kidney disease (32%). A third of the patients had pneumonia severity index (PSI) class IV with the rest approximately evenly distributed across the other four classes.
The median time to clinical stability was significantly shorter in the prednisone group than in the placebo group: 3.0 days versus 4.4 days, respectively, with a hazard ratio (HR) of 1.33 (95% Confidence interval (CI):1.15 to 1.50; p<0.0001). Among the secondary endpoints, time to discharge (6.0 days vs 7.0 days; p=0.012) and IV antibiotic days (4.0 vs 5.0; p 0.011), were the only variables with statistically significant improvements favoring the prednisone group. Pneumonia-associated complications were less in the prednisone group, but the difference just missed statistical significance with odds ratio (OR): 0.49 (CI: 0.23 to 1.02; p= 0.056). These improvements came at the cost of an increased rate of steroid-associated adverse events, mostly driven by a statistically significant in-hospital hyperglycemia requiring new insulin treatment that largely resolved by day 30.
The authors specified pre-defined interaction variables (age, initial C-reactive protein concentration, history of COPD, PSI class and blood culture positivity) to address possible effect modification, which was not found in the statistical analysis. This suggests that the higher risk patients within the study – those with older age and PSI class IV and V, for example, did not account for the majority of the difference seen.
What were the flaws of the study?
There are a number of issues regarding the reported baseline characteristics of each patient group. First, active smoking, prior pneumonia and pneumonia vaccine status were not addressed in baseline characteristics. If differential rates of these variables were found between the study and control groups the statistical analysis should have accounted for that difference. Second, approximately 23% of patients had “antibiotic pretreatment.†This was not defined in the text of the paper and might suggest that this sub-group of patients may have different pathogens or possibly met criteria for healthcare-associated pneumonia.
The effect of culture data on the study results was also lacking. The full methods, published separately[10], noted that initial laboratory assessment of all patients included Legionella and pneumococcal urine antigens. These data were not presented in the final manuscript. The study appendix lists the microbiological etiology of CAP, which was available in about 20% of the enrolled patients without differences between groups. It does not appear that the effect of any particular isolated microorganism on study outcomes was evaluated. This is important because the clinical benefit of steroids in meningitis appears to be more useful in cases caused by Streptococcus pneumoniae than those caused by Neisseria meningitidis.[11] Acknowledging that it is easier to get reliable microbiological data from cerebrospinal fluid culture than sputum samples, perhaps the clinical benefits of prednisone in these CAP patients may be driven by prevalence of pneumococcal pneumonia. If so, we might be able to prevent unnecessary adverse effects of glucocorticoids in a subset of CAP patients where there is no proven benefit of steroids. That said, blindness to precise microbiologic diagnosis mimics usual clinical practice.
Finally, it should be noted that all patients in this study were hospitalized, limiting our ability to extrapolate these results to ambulatory settings and those discharged from the emergency department.
What is the bottom line?
The results of the STEP trial are important additions to the canon of existing research in this field. Not only did they enroll a large number of patients across all PSI classes, but they also chose a clinically important primary endpoint for patients with moderate-severity pneumonia where the risk of death and serious adverse reactions are lower.[12] Three months after the STEP trial was published in the Lancet a systematic review and meta-analysis by Siemieniuk et al was published in Annals of Internal Medicine that included the STEP study and one other recently published study that used adjunctive steroids exclusively in severe CAP. [13,14]  The results of Siemieniuk et al’s analysis demonstrated a shorter time to clinical stability and shorter duration of hospitalizations in patients with CAP treated with adjunctive steroids with high certainty. The STEP study provided the power to make that claim.
Adjunctive corticosteroids are the standard of care for a number of other infections including bacterial meningitis, pneumocystis pneumonia and acute viral hepatitis.[15] The results of the STEP study suggest that it is time we add CAP to this list.
Is this study a Game Changer?Â
We asked Dr. Harald Sauthoff, Associate Professor of Medicine and Director of the Medical Intensive Care Unit at VA New York Harbor Healthcare System his opinion on how this trial fits into clinical practice.Â
Whether steroids can improve the outcome of patients with community-acquired pneumonia is an old question that has been unresolved for decades. The publication of two new randomized trials in 2015 [9, 10] and 3 recent meta-analyses [5, 6,13] has reinvigorated the debate. The currently available data suggest that the addition of steroids to standard therapy seems to shorten the time to clinical stability, but does not improve survival in the overall population. A mortality benefit may be present in a subgroup of patients with severe pneumonia. As always, one size does not fit all, and a lot still has to be learned about which patient population will benefit most from the addition of steroids. Do we treat bacterial and viral pneumonia the same? Do we need to target specific organisms, as for the treatment of meningitis? In addition, we need to better understand what differentiates inflammation that is beneficial to fight infection from an inflammatory response that leads to organ dysfunction. Eventually, this could lead to a well-timed and more individualized treatment approach. The recently published studies have swung the pendulum more towards steroids in patients with pneumonia, but we still have to learn a lot more before we can win the game.
Dr. Martin Fried is an internist at NYU Langone Medical Center
Peer reviewed by Harald Sauthoff, Pulmonary Medicine at NYU Langone Medical Center
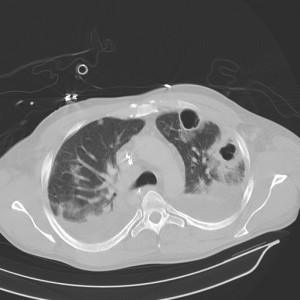
Image courtesy of Wikimedia Commons
References
[1] Marrie, Thomas J., and Jane Q. Huang. “Epidemiology of community-acquired pneumonia in Edmonton, Alberta: an emergency department-based study.” Canadian respiratory journal: journal of the Canadian Thoracic Society 12.3 (2005): 139-142. https://www.hindawi.com/journals/crj/2005/672501/abs/
[2] Angus, Derek C., et al. “Epidemiology of severe sepsis in the United States: analysis of incidence, outcome, and associated costs of care.” Critical Care Medicine-Baltimore- 29.7 (2001): 1303-1310.
[3] Wagner Jr, Henry N., et al. “The effect of hydrocortisone upon the course of pneumococcal pneumonia treated with penicillin.” Bulletin of the Johns Hopkins Hospital 98.3 (1956): 197-215. https://www.ncbi.nlm.nih.gov/pubmed/13304518
[4] Siempos, Ilias I., et al. “Adjunctive therapies for community-acquired pneumonia: a systematic review.” Journal of antimicrobial chemotherapy 62.4 (2008): 661-668. https://www.ncbi.nlm.nih.gov/pubmed/18641037
[5] Chen, Yuanjing, et al. “Corticosteroids for pneumonia.” Cochrane Database Syst Rev 3 (2011).
[6] Shafiq, Majid, et al. “Adjuvant steroid therapy in communityâ€acquired pneumonia: A systematic review and metaâ€analysis.” Journal of Hospital Medicine 8.2 (2013): 68-75.
[7] Snijders, Dominic, et al. “Efficacy of corticosteroids in community-acquired pneumonia: a randomized double-blinded clinical trial.” American journal of respiratory and critical care medicine 181.9 (2010): 975-982. https://www.ncbi.nlm.nih.gov/pubmed/20133929
[8] Meijvis, Sabine CA, et al. “Dexamethasone and length of hospital stay in patients with community-acquired pneumonia: a randomised, double-blind, placebo-controlled trial.” The Lancet 377.9782 (2011): 2023-2030.
[9] Blum, Claudine Angela, et al. “Adjunct prednisone therapy for patients with community-acquired pneumonia: a multicentre, double-blind, randomised, placebo-controlled trial.” The Lancet 385.9977 (2015): 1511-1518. http://thelancet.com/journals/lancet/article/PIIS0140-6736(14)62447-8/abstract
[10] Blum, Claudine A., et al. “Corticosteroid treatment for community-acquired pneumonia—the STEP trial: study protocol for a randomized controlled trial.”Trials 15.1 (2014): 257.
[11] De Gans, Jan, and Diederik Van de Beek. “Dexamethasone in adults with bacterial meningitis.” New England Journal of Medicine 347.20 (2002): 1549-1556.
[12] Valencia, Mauricio, et al. “Pneumonia severity index class v patients with community-acquired pneumonia: characteristics, outcomes, and value of severity scores.” CHEST Journal 132.2 (2007): 515-522. https://www.researchgate.net/publication/41454591_Pneumonia_severity_index_Class_V_patients_with_community-acquired_pneumonia_characteristics_outcomes_and_value_of_severity_scores_2007
[13] Siemieniuk, Reed AC, et al. “Corticosteroid therapy for patients hospitalized with community-acquired pneumonia: a systematic review and meta-analysis.” Annals of internal medicine 163.7 (2015): 519-528. http://annals.org/aim/article/2424872/corticosteroid-therapy-patients-hospitalized-community-acquired-pneumonia-systematic-review-meta
[14] Torres, Antoni, et al. “Effect of corticosteroids on treatment failure among hospitalized patients with severe community-acquired pneumonia and high inflammatory response: a randomized clinical trial.” JAMA 313.7 (2015): 677-686.
[15] Aberdein, Jody, and Mervyn Singer. “Clinical review: a systematic review of corticosteroid use in infections.” Critical Care 10.1 (2005): 203. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1550829/