 By Priya Patel, MD
By Priya Patel, MD
Peer Reviewed
This last week, ISIS had a number of terrorist attacks, confirming a shift from traditional battlefield tactics back to targeted attacks seen prior to 2014. They …

 By Priya Patel, MD
By Priya Patel, MD
Peer Reviewed
This last week, ISIS had a number of terrorist attacks, confirming a shift from traditional battlefield tactics back to targeted attacks seen prior to 2014. They …
 By Tania Ruiz-Maya, MD
By Tania Ruiz-Maya, MD
Peer Reviewed
This past week there was great news for all animal advocates and conservationists when the world’s largest chimpanzee research facility, Louisiana’s New Iberia Research Center (NIRC), announced …
 By Nydia Ekasumara, MD
By Nydia Ekasumara, MD
Peer Reviewed
Fighting resumes in Syria as an air strike hit the Al Quds hospital in the divided city of Aleppo, killing 27 people including children and …
 By: Scott Statman, MD
By: Scott Statman, MD
 Peer Reviewed
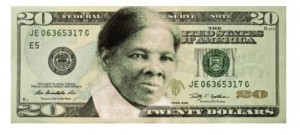
The widely anticipated New York State presidential primaries were held this past Tuesday. In the Democratic contest Hilary Clinton won a 60% majority, solidifying her commanding lead …
 By B. Corbett Walsh, MDÂ
By B. Corbett Walsh, MDÂ
Peer Reviewed
As many of us reflect on the Democratic Presidential Debate held this past Thursday in our backyard in Brooklyn, we prepare for the New York Primary …
 By Neha Jindal, MD
By Neha Jindal, MD
Peer Reviewed
Pharmaceutical companies made headlines last week when the $150 billion Pfizer-Allergan merger was called off shortly after the Obama administration issued new rules designed to …
 By Ajay Prakash, MD
By Ajay Prakash, MD
Peer Reviewed
Another week, and the Republican Primary continues to provide significant political intrigue. Donald Trump’s national [1] and primary [2] poll numbers collapse in the wake of a …
 By Vaughan Tuohy, MD
By Vaughan Tuohy, MD
Peer Reviewed
This week saw the beginning of March Madness [1]Â with major upsets by 15-seed Middle Tennessee over 2-seed (and perennial contender) Michigan State, Hawaii over California, Stephen F. …