 By Joseph Plaksin
By Joseph Plaksin
Peer Reviewed
This week, the Senate Intelligence Committee declassified a 500-page report that outlined and described uses of torture by the CIA to interrogate suspected terrorists …

 By Joseph Plaksin
By Joseph Plaksin
Peer Reviewed
This week, the Senate Intelligence Committee declassified a 500-page report that outlined and described uses of torture by the CIA to interrogate suspected terrorists …
 By Amar Parikh, MD
By Amar Parikh, MD
Peer Reviewed
This week, the nation was rocked by the decision of a Staten Island grand jury to not indict Officer Daniel Pantaleo in the death of …
 By Matthew Weiss, MD
By Matthew Weiss, MD
Peer Reviewed
Background:
The number of worldwide air travelers is expected to surpass 3.3 billion by 2015 and possibly double by 2030 [1]. These changes …
 By Chio Yokose, MD
By Chio Yokose, MD
Peer Reviewed
As temperatures took a noticeable dip earlier this week in New York City, prompting many of us to begrudgingly pull out our heavy down coats …
 By Max Padgett, MD, MPH
By Max Padgett, MD, MPH
Peer Reviewed
The United States and China, the two largest producers of greenhouse gases, have reached a historic agreement on reducing carbon emissions. President Obama announced …
 By Shannon Chiu, MD
By Shannon Chiu, MD
Peer Reviewed
This past Tuesday’s midterm congressional elections proved to be a big day for the Republicans, as they took control of the Senate and a record number …
 By Benjamin Geisler, MD MPH
By Benjamin Geisler, MD MPH
Peer reviewed
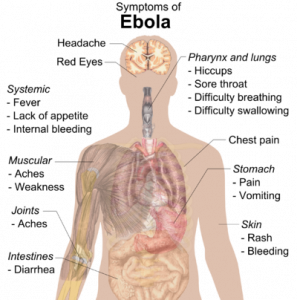
With the first Ebola patient being treated in the New York City area in one of our own training institutions, the viral …
 By Anish Parikh, MD
By Anish Parikh, MD
Peer Reviewed
This week, the Ebola virus outbreak continues to dominate the news both here and abroad. The number of newly-diagnosed patients in West Africa continues to …