 By Joshua Smith, MD
By Joshua Smith, MD
Faculty Peer Reviewed
CASE:Â A 54-year-old Asian female with no significant past medical history presents to her primary care physician with the complaint of several weeks …

 By Joshua Smith, MD
By Joshua Smith, MD
Faculty Peer Reviewed
CASE:Â A 54-year-old Asian female with no significant past medical history presents to her primary care physician with the complaint of several weeks …
 By Nelson Sanchez, MD and Fritz Francois, MD, MS
By Nelson Sanchez, MD and Fritz Francois, MD, MS
Faculty Peer Reviewed
Case: A 45-year-old woman presents to your office for an annual check-up. She states that her grandmother was …
 By Nicole Leigh Aaronson,MD,  Loren Wissner Greene, MD, and Denise Pate, MD
By Nicole Leigh Aaronson,MD,  Loren Wissner Greene, MD, and Denise Pate, MD
Faculty Peer Reviewed
Introduction:
Whereas there are specially designed diets for patients with hypertension, diabetes, and …
 By Mary C. Whitman, MD
By Mary C. Whitman, MD
Faculty Peer Reviewed
Proton pump inhibitors (PPIs) are generally considered “safe†medications[1] and are prescribed to over 100 million patients per year for a variety of indications, often …
 Nathaniel Rosso Smilowitz, MD
Nathaniel Rosso Smilowitz, MD
Faculty Peer Reviewed
Hepatitis B virus is a DNA hepadnavirus affecting 1.25 million people in the United States and nearly 400 million worldwide. The virus …
 By Lara Dunn, MD
By Lara Dunn, MD
Faculty Peer Reviewed
In 1958, EC Heyde published 10 cases of aortic stenosis (AS) and arteriovenous malformations (AVMs) of the gastrointestinal tract in the …
 By Todd Cutler
By Todd Cutler
Faculty Peer Reviewed
A 31-year-old woman presents to the clinic with chronic fatigue. She was diagnosed with iron  deficiency anemia when she was 25 …
 By Ramya Srinivasan, MD
By Ramya Srinivasan, MD
Faculty Peer Reviewed
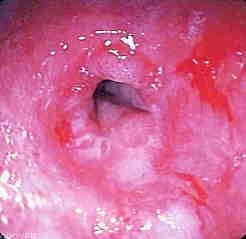
The patient is a 29 year old overweight male presenting to clinic with complaints of reflux symptoms. He says that spicy foods aggravate these symptoms. In …