 A 58 year old man with type 2 diabetes and chronic venous insufficiency/recurrent lower extremity cellulitis presents with fever and a left lower extrmity ulcer with purulent drainage. He’s been successfully treated in the past with both Unasyn/Augmentin or Levaquin. In the face of community acquired methicillin resistant staph aureus (CA-MRSA), have guidelines for skin and soft tissue infections changed?
A 58 year old man with type 2 diabetes and chronic venous insufficiency/recurrent lower extremity cellulitis presents with fever and a left lower extrmity ulcer with purulent drainage. He’s been successfully treated in the past with both Unasyn/Augmentin or Levaquin. In the face of community acquired methicillin resistant staph aureus (CA-MRSA), have guidelines for skin and soft tissue infections changed?
Commentary By Howard Leaf, M.D. Assistant Professor, Division of Infectious Diseases and Immunology
1. What would your first line treatment be in a patient with a diabetic ulcer?
Although New York City was not in the vanguard of regions reporting very high rates of CA-MRSA (Bellevue’s rate for S. aureus isolates from purulent skin and soft tissue infections in August 2004 was 15%; NEJM 2006; 355:666), we’re no doubt catching up. A study from hospitals in Brooklyn (Ann Clin Microbiol Antimicrob 2006; 5:29) reported 22% of all S. aureus isolates from 12/05 to 2/06 were positive for SCCmec type IV (the genetic element encoding resistance in most CA-MRSA), with many of these the most common USA-300 strain.
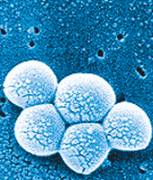
How does this impact your management of the diabetic foot ulcer? Given the above rates and the fact that S. aureus remains the most common pathogen isolated from diabetic associated ulcers, coverage of this pathogen would seem reasonable for moderate to severe ulcers as empiric therapy, pending cultures. This approach was reflected in the 2004 Infectious Diseases Society of America (IDSA) guidelines (Clin Infect Dis 2004;39:885-910). However, although some smaller series report diabetics as a risk for CA-MRSA acquisition, and perhaps poorer outcomes with disease, the usual scenario for this pathogen is epidemic furunculosis or other purulent complicated skin and soft tissue infections, not the typical diabetes associated ulcer.
Clindamycin has excellent antistaphylococcal activity, but there is the potential for emergence of resistance with strains inducibly resistant to erythromycin. Linezolid, daptomycin, and vancomycin have good efficacy in skin and soft-tissue infections and are choices as empiric therapy in the more severe infections in hospitalized patients. Over 95% of CA-MRSA isolates retain susceptibility to trimethoprim-sulfamethoxazole, and this has been used successfully. A fluoroquinolone (FQ) such as levofloxacin or moxifloxacin may also be chosen, but beware the possibility of emergence of resistance with prolonged therapy. The bottom line: for outpatient therapy, TMP-SMX plus either a fluoroquinolone or amoxicillin-clavulanate, or in more severe ulcers, linezolid plus a FQ. In the hospitalized patient, our old standby of vancomycin plus piperacillin-tazobactam is excellent coverage, with substitutions for either of those available.
2. What would your first line rx be in a diabetic patient with a routine cellulitis who you are treating as an inpatient?
Non-purulent cellulitis without an open wound in DM is usually due to β-hemolytic streptococci (A, B, C, and G) and less commonly S. aureus. Always consider necrotizing cellulitis requiring surgical debridement. Again, vancomycin or linezolid plus piperacillin-tazobactam or a carbapenem are appropriate for a patient with severe disease. For more mild infections, oral TMP-SMX plus linezolid or rifampin should do.
3. What would your first line rx be in a non-diabetic patient with a routine cellulitis who you are treating as outpatient? Should it include CA-MRSA coverage in the VA population? at Bellevue?
If “routine” is meant to connote lack of purulence or evidence of deep infection in a patient without some stronger epidemiologic link to CA-MRSA, such as a child, a prisoner, an MSM, a younger non-white patient, or the “classic” patient involved in team contact sports, amoxicillin-clavulanate or dicloxacillin may still be adequate. Otherwise, the addition of TMP-SMX is prudent, no matter the hospital at which you’re seeing your patient.

One comment on “Does the Existence of Community Acquired MRSA Change Empiric Therapy for Skin and Soft Tissue Infections?”
1. In the quoted NEJM paper Bellevue ER rates of MRSA are so out of sync with all the other sites and the number of patients is so small (20), that I cannot help but question the validity of data collection/case identification at that study site.
2. Though generally safe, hypersensitivity to bactrim is not as rare as one may hope. Bellevue’s MRSA (at least hospital isolates for which we have data) seems to be sensitive to tetracyclines more than 90% of the time. Any comment on using these drugs for PO management?
3. Since diabetics are probably not at high risk for community MRSA and since DM wound infection is not a typical presentation of the bug, why not simply use PO dicloxacillin or Augmentin in a stable patient while waiting for the cultures?
4. I am personally not a big fan of new Abx as long as older once retain activity. I have a serious mental block even considering either Linezolid or daptomycin in patients without contraindications to vancomycin.
Comments are closed.