 Commentary by Melissa Freeman MD, PGY-2
Commentary by Melissa Freeman MD, PGY-2
A 30 year-old male resident presents to his primary care physician for a routine physical examination. A small, nontender left-sided scrotal mass is felt. The patient states that this asymptomatic mass has been present for one year and was evaluated by a prior physician who felt that further work-up was unnecessary. He is sent for a testicular ultrasound which reveals a grade II varicocele. His testosterone level was low and he later had a semen analysis which was abnormal.
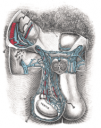
Present in 15% of post-pubertal males, varicocele is an abnormal dilatation of the pampiniform plexus of the scrotal veins. It is most common in young boys and, as such, the acute development of varicocele in the older patient should prompt further evaluation. With the patient standing, the scrotum should be inspected for visible distention around the spermatic cord. The physician should then palpate for a mass, often described as a “bag of worms”. Varicoceles can be graded from I, small and palpable only with the Valsalva maneuver which distends the pampiniform plexus, to III, large and visible on gross palpation.
Varicocele maintains a left-sided predominance due to the anatomy of the left renal vein compared to the right. 33% of patients are found to have them bilaterally and interestingly up to 40% of men with a palpable left varicocele may actually have bilateral varicoceles that are not initially discovered. A unilateral right varicocele is extremely rare and should lead to an investigation of IVC obstruction. They are often asymptomatic and benign but can cause anything from a dull discomfort (often greater while standing) to a very sharp pain. More importantly, varicocele can be a cause of male infertility and testicular atrophy.
Roughly, 40% of men undergoing evaluation for infertility are diagnosed with varicocele, yet there is a hazy, imprecise relationship between varicoceles and infertility. Despite studies spanning decades, the exact pathophysiology of how infertility results from varicocele remains poorly defined. It is believed that the venous dilation caused by varicocele leads to impaired intra-testicular circulation/heat exchange resulting in an elevated intra-testicular temperature. This negatively affects the Sertoli cells and spermatozoa. The decline in semen parameters and testosterone may be duration-dependent. Research also points to the possibility of Leydig cell dysfunction with a resultant decrease in testosterone biosynthesis as well as temperature-related enzymatic impairment in the steroid pathway of testosterone. Both can result in impaired semen quality. Though the details are beyond the scope of this article, it should be noted that a myriad of intriguing studies have proposed alternative pathophysiological mechanisms to explain how infertility can result from varicocele. These include reflux of renal or adrenal metabolites from the renal vein, hypoxia with or without excessive production of reactive oxygen species, altered levels of Fas and Fas-ligand expression leading to apoptosis of germ cells, and intra-testicular hyperperfusion injury with possible anti-sperm antibody production. Lastly, it is hypothesized that testicular atrophy secondary to varicocele is caused by increased scrotal temperature leading to apoptosis induction and an ultimate loss of germ cell mass.
Established treatment guidelines for varicocele in the adult population are poorly defined leaving treatment decisions to the discretion of the physician. Many urologists base their clinical decisions on the results of their histories, physical examination, and semen analyses. In the adult male with new varicocele, rare, but serious conditions like renal cell carcinoma, IVC thrombus, or right renal vein thrombosis should be considered. Regardless of symptoms, a semen analysis should usually be obtained in the young male to evaluate sperm quality and quantity. A testosterone level may also be obtained. Treatment of varicocele in young men with testicular atrophy or testicular growth retardation is generally indicated. In young men who have not yet completed their families, the semen analysis and a history of infertility are important to review. Without a history of infertility, if the semen analysis and testosterone are within normal limits, conservative treatment consisting of observation, NSAIDs, or scrotal elevation is likely all that is necessary. If the semen analysis is abnormal, surgical consideration is warranted. Surgical options for varicolcele include varicocelectomy, which is a ligation of the spermatic or gonadal vein, or radiologic embolization, which is an alternative with a higher risk:benefit ratio.
Numerous studies have compared semen analysis and hormonal levels before and after varicolectomy in patients with infertility to post-operative benefits. The highly variable study results have created the great contention of whether these interventions actually repair infertility. In their Cochrane Review, Evers et al. (2001) found that it is largely the uncontrolled versus the controlled studies that report improvement in semen qualities following varicocele ligation. Still, this meta-analysis is flawed by omitted inclusion criteria. In contrast, in their randomized controlled study, Magdar et al. (1995) showed that varicocelectomy is an effective treatment for male subfertility. Patients with larger varicoceles have been found to have better surgical outcomes in terms of improved semen analysis than those patients with smaller varicoceles. Multiple studies have also showed that testosterone production improves after surgical intervention. It has also been pointed out that patients may have undiagnosed bilateral varicoceles accounting for why a unilateral varicocelectomy may not improve semen quality and testosterone levels in the negative studies.
Returning to our clinical case, it is important to carry out a proper testicular exam and provide appropriate attention to any abnormalities. One must be aware of the relationship between varicocele and infertility and decide whether simple observation or surgery is needed. The young man in the case was evaluated by a urologist who recommended that he undergo a varicelectomy; he is scheduled to have the procedure this month.
References:
Costanzo, Linda. Physiology. Saunders co, Philadelphia, 2002.
Evers, JL, Collins, JA, Vandekerckhove, P. Surgery or embolization for varicocele in subfertile men (Cochrane review). Cochrane Database Syst Rev 2001; 1:CD000479
Eyre, Robert C. Evaluation of nonacute scrotal pathology in adults @ UpToDate.com, accessed 12/30/07.
Gat Y, Bachar GN, Zukerman Z, Belenky A, Gornish M. Varicocele: a bilateral disease. Fertil Steril. Feb 2004; 81(2):424-9.
Hooman, D, Abdolorasol, M, Modjtaba, R, Djaladat, Y, Pourmand, G. Varicocele and Antisperm Antibody: Fact or fiction? Southern Medical Journal, 99 (1), Jan 2006; pp 44-47.
Madgar I, Weissenberg R, Lunenfeld B, Karasik A, Goldwasser B. Controlled trial of high spermatic vein ligation for varicocele in infertile men. Fertil Steril. Jan 1995;63(1):120-4.
Schiff, J., Ramirez, M., Natan, B., Medical and surgical management of male infertility. Endocrinol Metab Clin N Am 36 (2007) 313-331.
Sirvent, J. J., Bernat, R., Navarro, M.A., Rodriguez, J, Guspi, R, and Bosch, R. Leydig cell in idiopathic varicocele. Eur. Urol. 17: 257, 1990.
Shiou-Dheng Chen et al. 8-hydroxy-2’-deoxyguanosine in leukocyte dna of spermatic vein as a biomarker of oxidative stress in patients with varicocele. Journal of Urology, 172: 1418-1421, 2004.
Su, L., Goldstein, M., Schlegel, P. The effect of varicocelectomy on serum testosterone levels in infertile men with varicoceles. Am Urological Association, 154 (5), Nov 1995; pp 1752-1755.
“Varicoceles” @ urologyhealth.org
Image courtesy of Wikipedia

One comment on “A Brief Glance at the Relationship between Varicocele and Infertility”
ya, thereis definately relation betwween varicocele and infertility. bcos in varicocele blood supply of testis impaired. that lead to decreas sperm production. and on long term that may lead to infertility.
Comments are closed.