Posted by Vivian Hayashi MD and Robert Smith MD, Mystery Quiz Section Editors
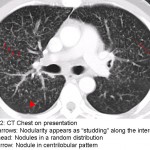
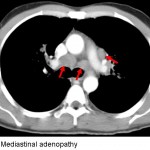
The answer to the mystery quiz is sarcoidosis. The CXR shows diffuse, bilateral infiltration with a predominantly nodular pattern. The pulmonary hila are also prominent. The CT image shows innumerable 2-3mm nodules, many of which have a perilymphatic distribution. The lymphatics, in parallel with the pulmonary vasculature, course through the interstitium. Hence, the perilymphatic nodularity has an interstitial distribution and appears as “studding” along the interstitium which is enhanced by vascular contrast (Image 2, short arrows). Additional nodules, however, have a random distribution (Image 2, arrowhead), while others appear to be centrilobular (Image 2, long arrow). As a granulomatous disease that involves activated CD4 lymphocytes, it is not surprising to find pathological involvement of perilymphatic tissue along with lymph nodes (Image 3, arrows). That said, sarcoidosis may involve any anatomical lung site: airways, interstitium or alveoli.
Perilymphatic nodularity also appears in the fissures and along the pleura where lymphatics are found (not shown). Other lung diseases included in the differential are also characterized by small nodules on chest imaging. Depending on their origin, the nodules have different distributions. Hematogenous spread of disease, such as miliary TB, will appear as interstitial disease because it is perivascular. Interstitial nodules due to miliary TB or metastatic disease, for example, appear to have sharp borders because they are enveloped by the interstitium which gives them a smooth edge on imaging. Nodules that arise from endobronchial spread of disease, such as aspiration or aerogenous spread of infection, often appear in a centrilobular distribution. The centrilobular location is where a bronchiole, filled with material conferring the appearance of a radiographic nodule, enters the lobule. The lobule appears as a polygonal structure (distal interstitium) on CT imaging. Beyond the bronchiole, nodules will manifest with a fuzzy border because they occupy airspace. Such nodules may also appear larger depending on how much neighboring airspace is involved.
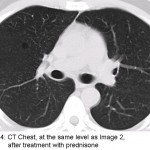
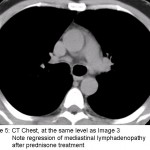
Our patient was treated with prednisone to alleviate his cough. His cough improved after a few weeks and repeat imaging showed regression of the pulmonary nodules (Image 4) and mediastinal lymphadenopathy (Image 5). Our case illustrates how patients with sarcoidosis often have imaging that is worse than would be expected from their clinical presentation.

One comment on “Mystery Quiz- The Answer”
Caption of image 3 should read mediastinal adenopathy
Comments are closed.