 David Shabtai
David Shabtai
Faculty Peer Reviewed
In a bold move, the U.S. Preventive Services Task Force recently changed their breast cancer screening guidelines – recommending beginning screening at age 50 and even then only every other year until age 75. Bold, because the Task Force members are certainly aware of the media circus that ensued when in 1997, an NIH group issued similar guidelines, prompting comparisons to Alice in Wonderland. The new guidelines, recommend “against routine screening mammography in women aged 40-49 years” as well as “concludes that the current evidence is insufficient to assess the additional benefits and harms of screening mammography in women 75 years or older.” Focusing on the younger group, the report clarifies that it applies only to women of average risk.
While the previous 2002 USPSTF recommendations encouraged screening mammography for women aged 40-49, new evidence has prompted the recent shift. Pooled meta-analysis showed that the risk reduction for breast cancer mortality in women aged 39-49 and 50-59 was almost identical, at 0.85 and 0.86 respectively. However, because of the lower incidence of breast cancer in the younger women, 1904 women needed to be screened so as to prevent 1 breast cancer related death in the 39-49 group, while only 1339 needed to be screened in the 50-59 group. During that decade of screening, each woman would be screened 2-9 times (requiring approximately 10,000 screenings to save one life). [As a reference, for women aged 60-69 – who have the highest incidence of breast cancer – 1 breast cancer death can be prevented with only 377 mammograms.]
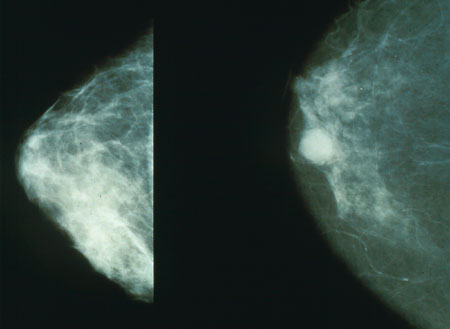
Implicit in those numbers is a cost benefit analysis. In terms of specific harms caused by routine mammography, most do not appear very drastic. 1. Radiation exposure is quite minimal – especially considering an additional aspect of the new USPSTF guidelines recommending mammography every 2 years instead of annually. 2. While certainly an unpleasant procedure, even described as painful, the report cites studies indicating that only a few women “would consider this a deterrent from future screening.” 3. Psychological factors, such as anxiety and distress, while significant, were almost always transient. Limitations to currently available testing and characteristics of the screening test itself however, lead to additional harms in terms of required follow-up testing. As a screening tool, mammography has a low rate of false negatives [0.1% in women aged 40-49 and 0.11% in women aged 50-59], but a more significant rate of false positives [9.78% in the younger group and 8.86% in the older group]. Traditionally, it is assumed that mammograms have a sensitivity of about 80%. Positive or questionable results on a screening mammogram require additional imaging and possibly even biopsy, which even then may be negative. Thus, for every 1000 women screened aged 40-49, 84.3 will require additional imaging and 9.3 will require biopsy. Only 1.8 of those 1000 women will end up with screening-detected invasive cancer. For the 50-59 group, 75.9 women will require additional imaging and 10.8 women will undergo biopsy to ultimately catch 3.4 out of the original 1000 women with screening-detected invasive cancer.
Based on these numbers, the USPSTF recommended against routinely screening women aged 40-49 but encouraged screening women aged 50-59. Considering that the main harms of screening are the necessary follow-up steps, the main question is whether the benefits of screening women aged 40-49 are really worth the effort. The USPSTF determined that they are not. In doing so however, they do not really explain how they came to this decision. Given their endorsement of routinely screening women aged 50-59, what separates that group from their younger cohort? For each 1000 women invited for screening, 1.6 additional women will have screening-detected breast cancer in the older group than in the younger group. 1.6 women out of 1000 are somewhat of a small difference to influence screening recommendations. Even when taking necessary follow-up procedures into account, the differences are not that drastic. Out of those requiring biopsy, 30% of the older group will be diagnosed with invasive cancer, while ‘only’ 20% of the younger group will be given such a diagnosis; a difference small enough that should not influence policy. The focus in fact, is on the mortality benefit. To save one woman from breast cancer related death, 1904 women aged 40-49 must be screened whereas, given the increased prevalence of breast cancer with age, screening only 1339 women aged 50-59 will save one life. However, treatments for younger women are often more successful than for older women and thus a more appropriate focus would be detection of invasive cancer – for which the difference between the age groups is not as impressively significant.
In an attempt to acknowledge the lack of precision in arriving at these recommendations, the USPSTF concludes “the decision to start [screening] … before the age of 50 years should be an individual one and take patient context into account, including the patient’s values regarding specific benefits and harms.” But shouldn’t this be true of any screening program? Aren’t the “patient’s values” supposed to guide the decision to begin any diagnostic workup? The only difference here appears to be the lack of USPSTF “recommendation” to do so – seemingly affecting only the attitude of the provider, but not the content of the conversation that needs to be had with the patient regardless of their age.
What seems paramount – but ostensibly lacking – in this discussion is an analysis of a physician’s responsibility to individual patients and how those responsibilities are shaped, governed, and guided by policy recommendations. This is especially true when the policy recommendations depend on relative statistics – balancing harms and benefits in different groups. The harms are not greater for 40-49 year old woman than for their older counterparts, they are simply more prevalent, but coupled with the benefit of saving a life with a longer potential life expectancy. Generally, the medical establishment and society at large are willing to ‘go farther’ and take on greater risk and cost to treat, cure, and prevent disease as the potential life expectancy of a successful intervention increases. Breast cancer prevention should be no different. For an individual patient, 1 in 1339 may have the same meaning as 1 in 1904 and they may be willing to undertake the risk of additional follow-up. Where that line should be drawn, or even how to determine where that line should be, is a very personal decision – one that is indeed dependent on a patient’s values, ethics, and views on life – not dictated by a medical organization.
Hopefully, these new “Guidelines” will spur these precise discussions between patients and their providers – discussions relevant to all medical interactions, not just cancer screening.
David Shabtai is a fourth year medical student at NYU School of Medicine
Peer reviewed by Robert N. Link, MD Associate Professor of Medicine, Chief, Medical Service Bellevue Hospital
References:
Fletcher, SW. Whither scientific deliberation in health policy recommendations? Alice in the Wonderland of breast-cancer screening. N Engl J Med. 1997;336:1180-1183.
Nelson HD, Tyne K, Naik A, et al. Screening for breast cancer: An update for the U.S. Preventive Services Task Force. Ann Intern Med. 2009;151:727-37.
U.S. Preventive Services Task Force. Clinical guidelines: Screening for breast cancer: U.S. Preventive Services Task Force recommendation statement. Ann Intern Med. 2009;151:716-726.

4 comments on “Revisiting the USPSTF Breast Cancer Screening Guidelines: Ethics, and Patient Responsibilities”
Comments are closed.