Faculty Peer Reviewed
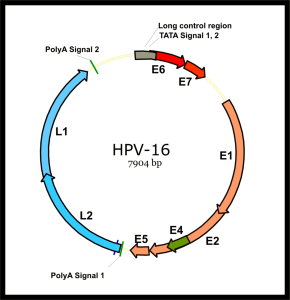
On December 22, 2010, the US Food and Drug Administration (FDA) approved the quadrivalent human papillomavirus (HPV) vaccine (Gardasil; Merck, Whitehouse Station, New Jersey) for prevention of anal cancer and anal intraepithelial neoplasia (AIN) for males and females 9 to 26 years old.[1] HPV is the most common sexually transmitted infection in the United States and the high-risk subtypes 16 and 18 are linked to development of cervical, vaginal, vulvar, anal, penile, and oropharyngeal malignancies. The FDA-approved uses for Gardasil have followed the epidemiological evidence linking HPV infection to a growing number of cancers in both males and females. The FDA originally approved the quadrivalent HPV vaccine in 2006 for cervical cancer prevention in females aged 9 to 26 years. In 2008, the FDA approved its use for the prevention of vaginal and vulvar cancers in the same population.[2] In 2009, the FDA approved its use in males and females from 9 to 26 years old for prevention of anogenital warts.[3]
Human papilloma virus DNA can be detected in the cervical tissue of 27% of women, according to the National Health and Nutrition Examination Survey, but can be found in up to 45% of women 20-24 years of age.[4] In men, the prevalence varies depending on the site sampled, but ranges from 20 to 65%.[5] In a group of HIV-negative men who have sex with men (MSM), 48% were infected with HPV; the high-risk HPV types 16 and 18 (associated with malignancy) were found in 13.7% and 8.1% respectively, and the low-risk types 6 and 11 (associated with anogenital warts) were detected in 13.4% and 6.8%. The strains for which the quadrivalent HPV vaccine is targeted–6,11,16, and 18–are found in the anal canal of 25.2% of men and 11.2% at penile sites.[6] The highest risk population, HIV-positive MSM, have a 95% rate of anogenital HPV infection.[6] Risk factors for anal HPV infection in MSM include 3-6 lifetime male sexual partners, younger age, and smoking. Males with 2 or more male lifetime sexual partners have a 3-4 times increased risk of anal HPV infection.[6]
The high prevalence of anogenital HPV infection in men, specifically in MSM, has led to a connection with both benign and malignant lesions. The low-risk HPV types 6 and 11 account for 90% of condyloma acuminata (genital warts) and the majority of HPV disease burden in men.[5] Penile cancer is uncommon, occurring in 8 out of 1 million men per year, but HPV 16 and 18 cause 40% of the roughly 1500 US cases per year. The incidence of anal cancer, rare in the general population (1/100,000), is increased 37 times in HIV-positive men and up to 100 times in HIV-positive MSM.[5] HPV type 16 causes 66% of anal cancer and type 18 causes 5%.[7] For the general population, the risk of anal cancer in men caused by HPV is much lower than that for cervical cancer in women, but in HIV-positive MSM, the incidence of anal cancer exceeds that of cervical cancer prior to screening programs.[8] HIV-positive patients are at increased risk for anogenital malignancy because of immunosuppression leading to reduced clearance of HPV and increased oncogenesis in cells co-infected with HPV and HIV.[12] The quadrivalent HPV vaccine is safe and effective in HIV-1-infected men, displaying seroconversion rates of 98%, 99%, 100%, and 95% for HPV types 6,11,16, and 18, respectively.[7]
Implementing widespread vaccination programs is a societal economic decision, relying on the cost per quality-adjusted life-year gained (QALY) compared to other prevention programs. Currently, the HPV vaccine is only routinely offered to females aged 9 to 26 because several studies have shown the HPV vaccine to be cost-effective at preventing cervical cancer in this population. A study by Kim and Goldie of the Harvard School of Public Health concluded that the cost of vaccinating 12-year old girls to prevent cervical cancer was $43,600 per QALY gained but rose to $152,700 per QALY when including females up to age 26.[9 ] When including the disease burden from genital warts caused by HPV, the cost per QALY was only reduced to $133,600. In another model including 12-year-old boys in the HPV vaccination program, Kim and Goldie concluded that the cost per QALY from cervical cancer prevention was $290,290 compared with vaccinating girls only; when including all HPV-related diseases in both sexes, it cost $120,000 per QALY.[10] Kim and Goldie therefore concluded that it is not cost-effective to expand widespread vaccination to boys compared to girls alone.[10] In contrast to these findings, a study by Elbasha and Dasbach of Merck & Co, the manufacturer of Gardasil, proposed that expanding the HPV vaccine indication to boys would only cost $25,664 per QALY for all HPV-related outcomes compared to only girls.[11] This vastly different result comes from different modeling procedures; the Merck model included the estimated diminished quality of life in women living with cervical intraepithelial neoplasia and used a higher vaccine efficacy (and included a full-page discussion debating the findings of Kim and Goldie).[10,11]
When specifically focusing on the prevention of anal cancer and anogenital warts in the high-risk population of men who have sex with men, the vaccination cost per QALY was only $15,290 for males at 12 years of age without exposure to HPV and $37,830 per QALY for MSM aged 26 with prior HPV infection.[8] Compared with the cost of cervical cancer prevention in women ($43,600 to $152,700 per QALY), vaccinating MSM for the prevention of anal cancer appears even more cost-effective. With the reduced rate of HPV clearance in HIV-positive individuals, it is important for physicians to recommend that MSM, especially those who are HIV-positive, receive the HPV vaccine to prevent anogenital malignancy. Whether or not to offer the vaccine to other low-risk male populations is debated among public health officials and policymakers. It is a philosophical and ethical question whether to offer the HPV vaccine to these low-risk males, who will obtain little if any benefit from vaccination themselves, for the goal of preventing disease in their future sexual partners.
Commentary by Andrew B. Wallach, MD, FACP
Prevention–both primary (preventing disease from occurring at all) and secondary (detecting asymptomatic disease early and preventing progression)–remains the crux of primary care. Kevin Burns succinctly summarizes the clinical and economic data surrounding HPV vaccination of men and boys. Of note, on October 25, 2011, the Advisory Committee on Immunization Practices (ACIP) voted to expand the routine use of quadrivalent HPV vaccine (HPV4). The expanded recommendations for HPV4 vaccination include:
• Routine vaccination of adolescent boys 11-12 years of age,
• Catch-up vaccination of males 13-21 years of age,
• Permissive use of vaccine among males 9-10 and 22-26 years of age, and
• Routine vaccination of men ages 22-26 who have HIV infection or who have sex with men.
ACIP also updated the federal Vaccines for Children (VFC) Program resolution for HPV vaccine to allow routine use and catch-up vaccination with HPV4 for VFC-eligible boys 9-18 years of age. As a result, in New York State, boys 9-18 years of age who are VFC-eligible or who are enrolled in Child Health Plus may receive publicly-purchased HPV4 in their medical homes. Boys 9-18 years of age who are considered “underinsured” under the State’s expansion provision of the VFC program may also receive the HPV4 in their medical homes. And, under New York Insurance Law, private insurance plans that are regulated by New York State are now required to cover HPV4 for boys 9-18 years of age. As Benjamin Franklin once stated, “an ounce of prevention is worth a pound of cure.”
Kevin Burns is a 4th year medical student at NYU School of Medicine
Peer reviewed by Andrew Wallach, MD, Department of Medicine (GIM Div), NYU Langone Medical Center
Image courtesy of Wikimedia Commons
References:
1. U.S. Food and Drug Administration. Gardasil approved to prevent anal cancer. http://www.fda.gov/newsevents/newsroom/pressannouncements/ucm237941.htm. Published December 22, 2010. Accessed January 27, 2011.
2. U.S. Food and Drug Administration. FDA approves expanded uses for Gardasil to include preventing certain vulvar and vaginal cancers. http://www.fda.gov/newsevents/newsroom/pressannouncements/2008/ucm116945.htm. Published September 12, 2008. Accessed January 27, 2011.
3. U.S. Food and Drug Administration. FDA approves new indication for Gardasil to prevent genital warts in men and boys. U.S. Food and Drug Administration. http://www.fda.gov/newsevents/newsroom/pressannouncements/ucm187003.htm. Published October 16, 2009. Accessed January 27, 2011.
4. Dunne EF, Unger ER, Sternberg M, et al. Prevalence of HPV infection among females in the United States. JAMA. 2007:297(8):813-819. http://jama.ama-assn.org/content/297/8/813.full
5. Barroso LF 2nd, Wilkin T. Human papillomavirus vaccination in males: the state of the science. Curr Infect Dis Rep. 2011;13(2):175-181.
6. Goldstone S, Palefsky JM, Guiliano AR, et al. Prevalence of and risk factors for human papillomavirus (HPV) infection among HIV-seronegative men who have sex with men. J Infect Dis. 2011:203(1):66–74. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3086446/
7. Wilkin T, Lee J, Lensing S, et al. Safety and immunogenicity of the quadrivalent human papillomavirus vaccine in HIV-1-infected men. J Infect Dis. 2010:202(8):1246-1253.
8. Kim JJ. Targeted human papillomavirus vaccination of men who have sex with men in the USA: a cost-effectiveness modelling analysis. Lancet Infect Dis. 2010:10(12):845-852.
9. Kim JJ, Goldie SJ. Health and economic implications of HPV vaccination in the United States. N Engl J Med. 2008:359(8):821-832.
10. Kim JJ, Goldie SJ. Cost effectiveness analysis of including boys in a human papillomavirus vaccination programme in the United States. BMJ. 2009:339:b3884.
11. Elbasha E, Dasbach E. Impact of vaccinating boys and men against HPV in the United States. Vaccine. 2010:28:6858-6867.
12.Vernon SD, Hart CE, Reeves WC, Icenogle JP. The HIV-1 tat protein enhances E2- dependent human papillomavirus 16 transcription. Virus Res. 1993;27(23):133-145.

2 comments on “Should Physicians Offer The HPV Vaccine To Men And Boys?”
I support male vaccination against the Human Papilloma Virus. They are the carriers of the virus and therefore if they are vaccinated against it they will greatly reduce the risk of cervical cancer in women.
Comments are closed.