Faculty Peer Reviewed
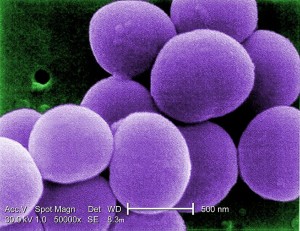
Staphylococcus aureus, first discovered in the 1880s, is one of the most widespread human pathogens. It is also a commensal organism, with about 20% of the population permanently colonized and 60% of the population intermittently colonized.[1] There is a wide variety of potential diseases that may develop when S aureus further invades the body, necessitating the use of antibiotics. Since the introduction of antibiotics into clinical practice, S aureus has developed unique ways to combat them. The evolution of S aureus resistance begins with the introduction of penicillin into clinical use in the mid 1940s, when it was routinely used for the successful treatment of S aureus. By the early 1950s, penicillin resistance had already developed and quickly became widespread.[2] Vancomycin, a compound first discovered from the organism Streptomyces orientalis on the island of Borneo, was approved for use in humans in 1958 but quickly fell by the wayside with the development of penicillinase-resistant methicillin in 1961. Methicillin-resistant S aureus (MRSA) developed rapidly, with the first strains isolated in less than a year and the first evidence of failed treatment in humans in 1968.[2,3] As MRSA strains became increasingly common, attention once again shifted to vancomycin, which saw a dramatic increase in use beginning in the early 1980s as it became the standard of care for MRSA.[4] Given the history of rapid development of methicillin resistance to S aureus, many feared the development of further resistance, and justifiably so, as vancomycin resistance has since been reported, beginning in 1997.[3]
Vancomycin-intermediate S aureus (VISA) is defined by the minimum inhibitory concentration (MIC) of 4-8 micrograms/milliliter in susceptibility testing.[5] Vancomycin-resistant S aureus (VRSA) is defined by any MIC higher than this. While these definitions make distinctions based on MIC alone, the mechanisms of resistance differ between the organisms in each resistance category.
The first vancomycin-resistant S aureus discovered was VISA, first identified in Japan in 1997.[3] The exact mechanism of resistance among VISA is not clear, but is thought to occur through an accumulation of various mutations that result in changes to the cell wall. One cell wall change that appears to be a universal characteristic is thickening.[6][7] Increased thickness of the cell wall is related to poor cross-linking, which leads to an excess of precursors with D-Ala-D-Ala termini, the peptidoglycan targets of vancomycin. These termini are able to bind the drug and prevent its diffusion to sites of synthesis at the inner aspect of the cell wall.[6,8] Interestingly, resistance appears to require a greater utilization of cell resources than normal MRSA strains, which leads to a slower doubling time. Indeed, in a vancomycin-free environment, vancomycin-susceptible MRSA strains are selected for. Thus, the very mechanisms that protect these bacteria also decrease their ability to transmit from person to person.[7] However, there exists a subtype of VISA known as heterogeneous vancomycin-intermediate S aureus (hVISA) in which a small number of cells in any given colony maintain a more resistant phenotype while the vast majority do not. This allows for the overall population of cells to grow more rapidly and infect more readily while still maintaining a subset of resistant cells that are capable of surviving in the setting of vancomycin use. It is thought that up to 20% of MRSA isolates in some areas may display the hVISA phenotype.[9] Currently, recognition of hVISA suffers from a lack of standardized testing.[7] Simple MIC susceptibility tests are not adequate, and population analysis profiles or other nonstandardized methods must be used. These tests are available in some clinical microbiology labs by special request.
More recently, the first strain found to be fully resistant to vancomycin (vancomycin-resistant S aureus or VRSA) was isolated. The first clinical case of VRSA was reported in 2002 in a woman from southeast Michigan with multiple recurrent diabetic foot ulcers. This woman was noted to be co-infected with vancomycin-resistant Enterococcus faecalis (VRE) and MRSA. Subsequent cultures later revealed the development of a vancomycin-resistant strain of S aureus, which was found to have an identical VanA transposon sequence to the previously isolated E faecalis. Despite resistance to vancomycin, multiple other susceptibilities were reported for this organism and the patient was treated successfully.[10] The proposed mechanism for the development of VRSA from MRSA involves VanA transposon transmission from VRE. It is likely that this occurred by means of conjugation between MRSA and VRE, followed by transposition of the VanA element to the MRSA chromosome. VanA confers resistance as a result of d-Ala-d-Lac peptidoglycan precursors that vancomycin can’t bind to.[6] As of September 2011, there were 12 total reported cases of VRSA in the United States, none of which resulted from person-to-person transmission.[11,12]
Although there have been no major outbreaks of VRSA, the past cases present a serious concern for future strains with increased infectivity. VISA and, more specifically, hVISA already seem to be present within a large number of MRSA isolates. Keeping this threat in check will require a multidisciplinary approach from public health officials, pharmaceutical companies, and individual practitioners. On the horizon, new antibiotics including lipoglycopeptides such as dalbavancin, oritavancin, telavancin, and new cephalosporins such as ceftaroline and ceftobiprole show promise against resistant strains of S aureus.[9,12] Additionally, studies involving combination therapy to prevent further selection for mutants in cases of serious S aureus infections may be warranted. The CDC provides a testing algorithm for clinical laboratories in the diagnosis and reporting of VRSA.[5] However, techniques that improve and standardize the methods for recognizing hVISA are needed. Healthcare providers can best help prevent this emerging threat by rigorously adhering to infection control guidelines, including proper isolation techniques, use of antibiotics as indicated by best clinical practice, and a continued vigilance against both MRSA and VRSA.
Brian Stierman is a 3rd year medical student at NYU School of Medicine
Peer reviewed by Bo Shopsin, MD, Medicine (Infectious Disease), NYU Langone Medical Center
Image courtesy of Wikimedia Commons
References:
1. Kluytmans J, van Belkum A, Verbrugh H. Nasal carriage of Staphylococcus aureus: epidemiology, underlying mechanisms, and associated risks. Clin Microbiol Rev. 1997;10(3): 505-520. http://cmr.asm.org/content/10/3/505.long
2. National Institute of Allergy and Infectious Diseases. Methicillin-resistant Staphylococcus aureus history. http://www.niaid.nih.gov/topics/antimicrobialResistance/Examples/mrsa/pages/history.aspx Updated March 4 2008. Accessed December 20, 2011.
3. Labelle A, Kollef MH. Emergence of methicillin-resistant Staphylococcus aureus. PCCSU. http://www.chestnet.org/accp/pccsu/emergence-methicillin-resistant-staphylococcus-aureus Published November 3, 2008. Accessed December 20, 2011.
4. Levine DP. Vancomycin: a history. Clin Infect Dis. 2006;42(S1):S5-S12. http://cid.oxfordjournals.org/content/42/Supplement_1/S5.long
5. Centers for Disease Control and Prevention. CDC reminds clinical laboratories and healthcare infection preventionists of their role in the search and containment of vancomycin-resistant Staphylococcus aureus (VRSA). http://www.health.ri.gov/materialbyothers/201005CDCAdvisoryVRSA.pdf Updated May 2010. Accessed December 20, 2011.
6. Périchon B, Courvalin P. VanA-type vancomycin-resistant Staphylococcus aureus. Antimicrob Agents Chemother. 2009;53(11):4580-4587. http://aac.asm.org/content/53/11/4580.full
7. Cui L, Ma X, Sato K, et al. Cell wall thickening is a common feature of vancomycin resistance in Staphylococcus aureus. J Clin Microbiol. 2003; 41(1):5-14. http://jcm.asm.org/content/41/1/5.full
8. Fridkin SK. Vancomycin-intermediate and resistant Staphylococcus aureus: what the infectious disease specialist needs to know. Clin Infect Dis. 2001;32(1):108-115. http://cid.oxfordjournals.org/content/32/1/108.full
9. Howden BP, Davies JK, Johnson PDR, Stinear TP, Grayson ML. Reduced vancomycin susceptibility in Staphylococcus aureus, including vancomycin-intermediate and heterogeneous vancomycin-intermediate strains: resistance mechanisms, laboratory detection, and clinical implications. Clin Microbiol Rev. 2010; 23(1):99-139. http://cmr.asm.org/content/23/1/99.full
10. Chang S, Sievert DM, Hageman JC, et al. Infection with vancomycin-resistant Staphylococcus aureus containing the vanA resistance gene. N Engl J Med. 2003;348(14):1342-1347. http://www.nejm.org/doi/full/10.1056/NEJMoa025025
11. Hayakawa K, Marchaim D, Vidaillac C, et al. Prevalence of vancomycin-resistant Enterococcus faecalis in the region with the highest prevalence of vancomycin-resistant Staphylococcus aureus. Infect Control Hosp Epidemiol. 2011;32(9):922-924. http://www.jstor.org/stable/10.1086/661599
12. Zhanel GG, Rossnagel E, Nichol K, et al. Ceftaroline pharmacodynamic activity versus community-associated and healthcare-associated methicillin-resistant Staphylococcus aureus, heteroresistant vancomycin-intermediate S. aureus, vancomycin-intermediate S. aureus and vancomycin-resistant S. aureus using an in vitro model. J Antimicrob Chemother. 2011;66(6):1301-1305. http://jac.oxfordjournals.org/content/66/6/1301.full