Faculty Peer Reviewed
We give hope to patients with advanced kidney disease that a transplant will save them from their Monday, Wednesday, Friday trips to the dialysis unit. But how certain are we that they even qualify to be a recipient? And if they do, are they going to live long enough to get their new lease on life?
Kidney donation has received its fair share of publicity recently, from the allocation of organs to illegal immigrants[1] to Good Samaritans starting a chain of kidney transplants.[2] Despite efforts to recruit more donors, thousands of people continue to die while on the transplant list. The average mortality rate on the waiting list is 6% per year and, with most people waiting 3-4 years, almost a quarter won’t survive.[3] So what do you tell your patient when they ask you, “Doc, how much longer?” The best thing one can do is to give them the facts.
Traditionally, cadaveric kidneys were the mainstay of transplantation. As cadaveric donation continues to be inadequate to meet the needs of the growing waiting list, patients are becoming more receptive to the idea of accepting a kidney from a living donor. Living donor kidneys now represent 40% [4] of all kidney transplants and have not only decreased the waiting time for recipients, but have almost doubled graft survival from 10-11 years for a cadaveric kidney to 18-19 years for a living donor kidney.[5] Furthermore, outcomes have been similar even if the donor is unrelated to the recipient. One of the biggest hindrances to living donation is the recipient’s concern for the donor’s wellbeing after the nephrectomy. Improvements have made the surgical and medical risks for donors minimal. What used to be an open operation is now done laparoscopically, (0.0003% perioperative mortality risk) [4] with the donor discharged home in 2 to 3 days and back to work within 3 to 4 weeks.[5] As donors generally tend to be healthy, they do not require care by a nephrologist and can be managed and counseled by their primary care physicians. It is essential to fully inform donors of the potential complications, which are small, but not nil. While there is no increase in long-term mortality for donors, it appears that some subsets of donors such as African-Americans and obese patients are at increased risk of developing chronic kidney disease, end-stage renal disease, hypertension, and, in obese patients, diabetes. It is unclear, however, if and how much the nephrectomy contributes to their baseline risk of developing these conditions, and more long-term follow-up is needed.[4]
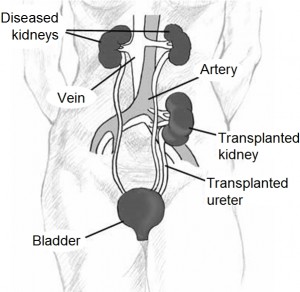
While the frequency of living donation is increasing, most patients still depend on cadaveric kidney transplantation, which involves a waiting list that is based primarily on optimal blood and antigen matching. While some aspects are out of the control of the physician, it is the responsibility of the physician to be the patient’s advocate and help them manage all variables that they can control.
The patient should be up to date on their health maintenance. As the patient’s primary physician, it is important to make sure that all labs and required screenings are completed before referral to a transplant unit (see Table).[6] Cardiology evaluation is most important, as that is the most common cause of exclusion from the transplant list. Patients with greater than 20% 10-year Framingham risk are deemed high-risk. All dialysis patients are automatically considered high-risk and should be screened every 2 years with stress testing for asymptomatic patients and coronary angiography for patients with symptoms of ischemia.[7] Patients with diabetes need annual reevaluation; it is now suggested that, given the insensitivity of stress testing in diabetic patients, their pre-transplant evaluation should include coronary angiography.[8]
| Table. Assessment of Renal Transplant CandidateSource: Modified from Pham et al: Semin Dial 23(6):595-605, 2010. |
| Laboratory evaluation |
| Serologies: HIV, hepatitis B and C, CMV, EBV, HSV, RPR (FTA-ABS if positive) |
| CMP, CBC with differential and platelet count, PT/INR, PTT |
| Urinalysis, urine culture |
| PSA in men >50 years of age (younger if at high risk of prostate cancer) |
| Immunofixation electrophoresis in candidates >60 years of age |
| Other evaluation |
| ECG |
| Chest X-ray |
| Colonoscopy if > 50 years of age |
| Abdominal ultrasound in diabetes to evaluate for gall stones |
| Native renal ultrasound to assess for acquired cystic disease or masses |
| Pap smear (for women) |
| Mammogram for women >40 years or with family history of breast cancer |
| Cardiac evaluation (see text) |
| Urological evaluation if history of bladder/voiding dysfunction, recurrent UTI |
| Immunologic studies |
| Blood group and HLA typing |
| HLA antibodies |
| Crossmatching |
The patient should be referred early. Ideally, people should get transplanted before dialysis is started. This is rarely the case, as most patients with chronic kidney disease don’t see a nephrologist until late in their disease. A number of variables have been noted to hinder a timely referral for transplantation. Physicians should be particularly attuned to patients with lower socioeconomic status, non-English-speaking backgrounds, and with obesity and diabetes.[9] Kidneys are allocated on a geographic level, starting locally and moving nationally. Patients who register at multiple units should be prepared to undergo extra medical testing and costs.
The patient should be patient. Assuming patients meet all the requirements listed above, they may be placed on the waiting list once they have started chronic dialysis or their glomerular filtration rate is less than 20 mL/min. In simplest terms, patients accrue one point for every year they are on the transplant list. Patients can also be bumped to the top of the list if a donor with a perfect human leukocyte antigen (HLA) match is found. Patients who are “highly sensitized” with panel-reactive antibodies that reject over 80% of donor antigens may receive 4 extra points, given the additional complexity of finding a donor. Patients may fall in this category if they have been pregnant, been the recipient of a prior transplant, or have received numerous blood transfusions. Limiting unnecessary transfusion is of prime importance. In some very rare situations, patients in danger of imminent death may qualify for “status 1.” In these instances, the transplant center may apply to the board of transplant physicians for “medical urgency” points to help the patient receive the next available organ. And finally, to propagate the “pay-it-forward” mantra, recipients who have donated a vital organ receive 4 additional points.[10]
The patient should (or should not) be picky about the kidney. Another discussion worth having with the patient is the risks and benefits of accepting an expanded criteria donor (ECD) kidney. These kidneys are of poorer quality, but the wait time is less compared to waiting for a standard donor kidney. In a study of patients receiving marginal kidneys, post-transplant life expectancy declined from 5.6 to 5.3 years but it only took 2 years to get the ECD kidney compared to 4 years for the standard kidney.[11] While this is a complex issue warranting a thorough discussion with the patient, data have clearly shown that patients over 40 with coexisting diabetes and in areas with long wait times (such as New York) benefit from ECD kidneys.[12]
The current guidelines and requirements differ depending on individual transplant units, but, in general, the entire system has room for improvement. The current system, heavily emphasizing time spent on the waiting list, will likely be transformed in the coming years to put more weight on life-years gained from transplantation (LYFT).[13] In the meantime, physicians can do their part by keeping their patients in good health and informed about all of their options. As mentioned, outcomes for living donor kidneys are better for the recipient, with only minimal risks for the donor. Patients should not shun the idea of living donor kidneys if that is an option for them.
Ilina Datkhaeva is a 3rd year medical student at NYU School of Medicine
Reviewed by Dr. Alexander Gilbert, Nephrology Medicine, NYU Langone Medical Center
Image courtesy of Wikimedia Commons
References:
1. Bernstein N. For illegal immigrant, line is drawn at transplant. New York Times. December 20, 2011. http://www.nytimes.com/2011/12/21/nyregion/illegal-immigrants-transplant-cheaper-over-life-isnt-covered.html?pagewanted=all Accessed March 21, 2012.
2. Sack K. 60 lives, 30 kidneys, all linked. New York Times. February 18, 2012. http://www.nytimes.com/2012/02/19/health/lives-forever-linked-through-kidney-transplant-chain-124.html Accessed March 21, 2012.
3. Gill JS, Rose C, Pereira BJ, Tonelli M. The importance of transitions between dialysis and transplantation in the care of end-stage renal disease patients. Kidney Int. 2007;71(5):442-447. http://www.nature.com/ki/journal/v71/n5/full/5002072a.html
4. Lentine KL, Patel A. Risks and outcomes of living donation. Adv Chronic Kidney Dis. 2012;19(4):220-228. http://www.ackdjournal.org/article/S1548-5595%2811%2900137-6/fulltext
5. McGill RL, Ko TY. Transplantation and the primary care physician. Adv Chronic Kidney Dis. 2011;18(6):433-438. http://www.ackdjournal.org/article/S1548-5595%2811%2900144-3/fulltext
6. Pham PT, Pham PA, Pham PC, Parikh S, Danovitch G. Evaluation of adult kidney transplant candidates. Semin Dial. 2010;23(6):595-605. http://onlinelibrary.wiley.com/doi/10.1111/j.1525-139X.2010.00809.x/full
7. Pilmore H. Cardiac assessment for renal transplantation. Am J Transplant. 2006;6(4):659-665. http://onlinelibrary.wiley.com/doi/10.1111/j.1600-6143.2006.01253.x/full
8. Welsh RC, Cockfield SM, Campbell P, Hervas-Malo M, Gyenes G, Dzavik V. Cardiovascular assessment of diabetic end-stage renal disease patients before renal transplantation. Transplantation. 2011;91(2):213-218.
9. Gaston RS, Danovitch GM, Adams PL, et al. The report of a national conference on the wait list for kidney transplantation. Am J Transplant. 2003;3(7):775-785. http://onlinelibrary.wiley.com/doi/10.1034/j.1600-6143.2003.00146.x/full
10. United Network for Organ Sharing. How the Transplant System Works. http://www.unos.org/donation/index.php?topic=fact_sheet_1. Accessed August 14, 2012.
11. Schold JD, Meier-Kriesche HU. Which renal transplant candidates should accept marginal kidneys in exchange for a shorter waiting time on dialysis? Clin J Am Soc Nephrol. 2006;1(3):532-538. http://cjasn.asnjournals.org/content/1/3/532.long
12. Merion RM, Ashby VB, Wolfe RA, et al. Deceased-donor characteristics and the survival benefit of kidney transplantation. JAMA. 2005;294(21):2726-2733. http://jama.jamanetwork.com/article.aspx?articleid=201963
13. Leichtman A, Stegall M. A dynamic period of reappraisal and innovation in kidney transplantation practice and policies. NephSAP. 2008; 7:1.