Faculty Peer Reviewed
Cannabinoid receptor agonists (CRAs) have been recently popularized as “legal” alternatives to marijuana and are becoming increasingly common, especially among teens and young adults. These new artificial “highs” consist of a blend of various dried herbs, spices and plant material that have been sprayed with one or more CRAs and are sold under names like Spice, K2, Mr. Smiley, Mr. Nice Guy, Black Mamba, Purple Haze, Spice Gold, and Smoke [1].
CRAs are thought to have first appeared in Germany around 2004 and the United States in 2008 [2]. Initially, the production and sale of CRAs were legal and unregulated, since most CRAs are structurally distinct from delta-9-tetrahydrocannabinol (THC), the active ingredient in marijuana. CRAs are often sold as incense and clearly labeled as “not for human consumption” or “for aroma therapy.” As a result, these products could be easily purchased through the Internet and at local gas stations, convenience stores, and smoke shops [1]. In a 2010 survey, 8% of the responding University of Florida students admitted to using CRA-containing products at least once [3]. It quickly became apparent that CRA abuse was becoming a significant public health problem as CRA-related calls to the American Association of Poison Control Centers increased from 53 calls in 2009 to over 6000 calls in 2011 [1]. On March 1, 2011, the US Drug Enforcement Administration issued a temporary ban of five of the more common CRAs, which was then made permanent on July 9, 2012. To further curtail the rise in CRA abuse, several states have implemented stricter laws against the production and sales of CRAs. While tests for a few of the more common CRAs are now available, the majority of CRAs are undetectable on routine urine drug screening. As a result, CRA use is thought to be popular in people subjected to routine drug screening, such as military personnel, firefighters, law enforcement officers, athletes, and airline pilots [4-6]. For example, one study showed that nearly 5% of all urine specimens collected from routinely screened US athletes tested positive for metabolites of two common CRAs, indicating recent use [6].
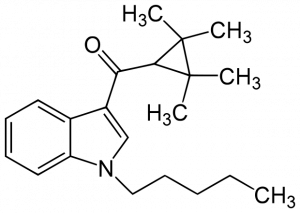
CRAs from the JWH family are the most commonly detected active compounds found in these new artificial marijuana products. These compounds were named after John W. Huffman, a National Institute of Drug Abuse-funded organic chemist, who created several synthetic CRAs in order to study the properties of THC in the early 1990s. Shortly afterwards, several additional CRAs were isolated from various products containing CRAs. In addition to the JWH series, there are three other groups of CRAs: the cyclohexylphenol (CP) compounds, the Alexandros Makriyannis (AM) compounds, and HU-210 (HU stands for Hebrew University) [1].
Research characterizing the effects of these CRAs in humans and animal models remains limited. CRAs, like THC, bind to and activate cannabinoid receptors. In contrast to THC, CRAs and their metabolites can also function as agonists, neutral antagonists, or inverse agonists at cannabinoid receptors [7-9]. There are two subtypes of cannabinoid receptors: CB1 and CB2 (CB1Rs and CB2Rs, respectively). CB1Rs are primarily found within the central nervous system and are responsible for the psychotropic effects that drive people to abuse THC; in contrast, CB2Rs are found primarily on peripheral immune cells and are involved in immune system suppression [10]. Compared with THC, JWH-018, the predominant CRA, has a 4-5- fold higher affinity for CB1R and CB2R. Additionally, it has been hypothesized that CRAs and their metabolites directly and indirectly target other receptors including both muscarinic and nicotinic acetylcholine receptors, serotonin receptors, GABA receptors, NMDA receptors, vanilloid type 1 receptor (TRPV1), and PPAR-alpha nuclear receptors [1,7-10]
Consumers buying a specific CRA-containing substance can never really know what they are actually purchasing. The content and concentration of CRAs vary considerably between and within brands. This is partly due to the fact that once a specific CRA is banned, it is often replaced by a newer CRA that has not yet been outlawed [11]. Moreover, “hot spots” or dosage variability within a single package are common [1]. In one study, 11% of the people surveyed reported variable and unpredictable responses with multiple uses of the same brand [12]. Additionally, little is known about the composition and effects of the organic plant material used in CRA-containing products; there are reports that some products contain adulterants, such as clenbuterol and excessive amounts of vitamin E [13]. Compared to THC, these additional pharmacologic properties endow CRAs with increased potency and a wider variety of physical and psychological effects.
Most people smoking CRAs report a positive, marijuana-like experience that lasts from 30 minutes to 2 hours [12]. Nevertheless, the medical literature contains several case studies of people who presented to emergency departments with serious CRA-related complications. The reported adverse effects include anxiety, restlessness, paranoia, psychosis, unresponsiveness, dystonia, dizziness, diaphoresis, tachycardia, hypertension, tachyarrhythmias, myocardial infarctions, and seizures [14-18]. There is at least one documented case of a patient who experienced CRA-associated dependence and withdrawal. The reported withdrawal symptoms were similar to those reported with marijuana withdrawal and included depression, tremor, palpitation, insomnia, headache, diarrhea, nausea, vomiting, tachycardia, and hypertension [19]. While the vast majority of patients with CRA toxicity recover without sequelae, very little is known about its long-term effects.
A thorough history about drug use and a high index of suspicion are important in diagnosing CRA abuse, as the presenting signs and symptoms of intoxication are often nonspecific and inconsistent. Most routine urine toxicology screening tests fail to detect recent CRA use and thus are of little clinical value. Therefore, CRA abuse must also be considered in any confirmed or suspected marijuana user who presents to the ED with symptoms inconsistent with traditional marijuana abuse, including but not limited to agitation, seizures, or acute, unexplained psychosis [20].
There are no specific antidotes for CRA intoxication. Therefore, a definitive diagnosis of acute CRA intoxication is not imperative, as treatment is largely supportive. In most cases, hydration and watchful waiting are sufficient for treatment, as the vast majority of CRA-related symptoms are self-limiting [20]. Benzodiazepines should be used in patients with agitation or seizures [15]. Antipsychotics, such as haloperidol, may be given to patients with psychosis. Initiation of advanced cardiac life support protocols is appropriate in patients with severe cardiac manifestations [16]. Patients with dystonia may be treated with diphenhydramine [18]. The National Poison Help Line (1-800-222-1222) is available 24 hours a day, 7 days a week to provide expert advice on treating suspected or confirmed CRA intoxication; the hotline also serves as a monitoring system to collect data on CRA abuse patterns.
Policy makers are faced with difficult decisions on how to deal with CRA abuse. As specific cannabinoid compounds are outlawed and become detectable in screening tests, a few things may happen. In the first scenario, newer compounds will be developed to skirt laws and detection, so the composition of CRA-containing products will continue to evolve and change. As the structures of these products are altered, their physiological and psychological effects will also likely change. This situation is problematic for researchers trying to characterize the acute and long-term effects of CRAs because a compound may become obsolete within the time a study is started and its publication. The second possible result of illegalization is that these products will begin to be produced and sold beside marijuana, crack, methamphetamine, and heroin on the illicit drug market. Obviously, neither option is desirable. An unorthodox alternative would be to legalize a few of the less potent cannabinoid compounds, including possibly THC itself, so that consumers have legal, but FDA-regulated, alternatives. The correct policy measure remains to be determined. As of yet, no one really knows if CRAs are here to stay, will die out, or will eventually evolve into something completely different. The story of CRAs is still in its infancy.
Ryland Pace is a 4th year medical student at NYU Langone Medical Center
Peer reviewed by Daniel Lugassy, MD, Medicine, NYU Langone Medical Center
Image courtesy of Wikimedia Commons
References
1. Seely KA, Lapoint J, Moran JH, Fattore L. Spice drugs are more than harmless herbal blends: a review of the pharmacology and toxicology of synthetic cannabinoids. Prog Neuropsychopharmacol Biol Psychiatry. 2012;39(2):234-243. http://www.ncbi.nlm.nih.gov/pubmed/22561602
2. European Monitoring Centre for Drugs and Drug Addiction. Early-warning system. Understanding the ‘Spice’ phenomenon. http://www.emcdda.europa.eu/attachements.cfm/att_80086_EN_Spice%20Thematic%20paper%20—%20final%20version.pdf. Published 2009. Accessed August 15, 2012.
3. Hu X, Primack BA, Barnett TE, Cook RL. College students and use of K2: an emerging drug of abuse in young persons. Subst Abuse Treat Prev Policy. 2011;6:16. http://www.ncbi.nlm.nih.gov/pubmed/21745369
4. Bebarta VS, Ramirez S, Varney SM. Complication of spice use in a deployed combat setting-seizure while on duty. Am J Addict. 2012;21(5):496-497. http://www.ncbi.nlm.nih.gov/pubmed/22882404
5. Johnson L, Johnson RL, Alfonzo C. Spice: a legal marijuana equivalent. Mil Med. 2011;176(6):718-720.
6. Heltsley R, Shelby MK, Crouch DJ, et al. Prevalence of synthetic cannabinoids in U.S. athletes: initial findings. J Anal Toxicol. 2012;36(8):588-593. http://www.unboundmedicine.com/evidence/ub/citation/22872465/Prevalence_of_synthetic_cannabinoids_in_U_S__athletes:_initial_findings_
7. Brents LK, Gallus-Zawada A, Radominska-Pandya R, et al. Monohydroxylated metabolites of the K2 synthetic cannabinoid JWH-073 retain intermediate to high cannabinoid 1 receptor (CB1R) affinity and exhibit neutral antagonist to partial agonist activity. Biochem Pharmacol. 2012;83(7):952-961.
8. Brents LK, Reichard EE, Zimmerman SM, Moran JH, Fantegrossi WE, Prather PL. Phase I hydroxylated metabolites of the K2 synthetic cannabinoid JWH-018 retain in vitro and in vivo cannabinoid 1 receptor affinity and activity. PLoS One. 2011;6(7):e21719.
9. Seely KA, Brents LK, Radominska-Pandya A, et al. A major glucuronidated metabolite of JWH-018 is a neutral antagonist at CB1 receptors. Chem Res Toxicol. 2012:25(4):825-827. http://www.ncbi.nlm.nih.gov/pubmed/22404317
10. Seely KA, Prather PL, James LP, Moran JH. Marijuana-based drugs: innovative therapeutics or designer drugs of abuse? Mol Interv. 2011;11(1):36-51.
11. Lindigkeit R, Boehme A, Eiserloh I, et al. Spice: a never ending story? Forensic Sci Int. 2009:191(1-3):58-63.
12. Vandrey R, Dunn KE, Fry JA, Girling ER. A survey study to characterize use of spice products (synthetic cannabinoids). Drug Alcohol Depend. 2012;120(1-3):238-241.
13. Wells DL, Ott CA. The “new” marijuana. Ann Pharmacother. 2011;45(3):414-417. http://www.ncbi.nlm.nih.gov/pubmed/21325097
14. Cohen J, Morrison S, Greenberg J, Saidinejad M. Clinical presentation of intoxication due to synthetic cannabinoids. Pediatrics. 2012;129(4):e1064-1067.
15. Lapoint J, James LP, Moran CL, Nelson LS, Hoffman RS, Moran JH. Severe toxicity following synthetic cannabinoid ingestion. Clin Toxicol (Phila). 2011;49(8):760-764.
16. Mir A, Obafemi A, Young A, Kane C. Myocardial infarction associated with use of the synthetic cannabinoid K2. Pediatrics. 2011;128(6):e1622-1627.
17. Schneir AB, Cullen J, Ly BT. “Spice” girls: synthetic cannabinoid intoxication. J Emerg Med. 2011;40(3):296-299.
18. Simmons J, Cookman L, Kang C, Skinner C. Three cases of “spice” exposure. Clin Toxicol (Phila). 2011;49(5):431-433.
19. Zimmermann US, Winkelmann PR, Pilhatsch M, Nees JA, Spanagel R, Schulz K. Withdrawal phenomena and dependence syndrome after the consumption of “spice gold”. Dtsch Arztebl Int. 2009;106(27):464–467.
20. Castellanos D, Thornton G. Synthetic cannabinoid use: recognition and management. J Psychiatr Pract. 2012;18(2):86-93. http://www.ncbi.nlm.nih.gov/pubmed/22418399
1