Faculty Peer Reviewed
It seems like a simple enough history: an 18 year old with a past medical history significant for GBS. They probably gave him some antibiotics for a Group B Strep infection and sent him home. Or did he need IVIG (that’s intravenous immunoglobulin) and plasmapheresis for Guillain-Barré syndrome? When a patient is prescribed MS will he receive morphine sulfate or magnesium sulfate? Abbreviations, used to save time and space, have become ubiquitous in prescriptions and medical records. However, they are frequently a source of confusion and can be a major risk in clinical practice. Medical students and doctors struggle with ambiguous abbreviations daily in trying to figure out a patient’s history from the chart. Although they can often be deciphered in context, these abbreviations can lead to serious morbidity and mortality. The United States Pharmacopeia MEDMARX program, a national medication error-reporting program used to report and track medication errors, found that of the 643,151 errors reported to them from 2004 through 2006, 4.7% were attributable to abbreviation use [1].
Effective communication between patient care team members is essential, and abbreviations can obfuscate what should be simple medical recommendations. A recent study of pediatric sign-out sheets at a large urban hospital found that, while pediatricians were able to understand 56-94% of the abbreviations used, physicians from other fields understood only 31-63%, highlighting the ambiguous nature of many abbreviations [2]. A similar study looked at a selection of abbreviations from recent hospital admissions and asked different members of a multidisciplinary care team to decipher them. They found that the average correct response rate was only 43%, again with specific abbreviations better known among the professionals who used them more frequently [3].
A recent study of three hospitals in Australia looked at lists of error-prone abbreviations in prescriptions from the National Coordinating Council for Medication Error Reporting and Prevention, the Institute for Safe Medications Practices, and the Joint Commission, and compared them to the abbreviations used in their hospitals. Of the 8296 medication orders they studied, 1162 error-prone abbreviations were found, with an average of 2.4 per patient [4]. With such widespread use of error-prone abbreviations and known morbidity as demonstrated by the MEDMARX program, there have been efforts at rectifying the problem.
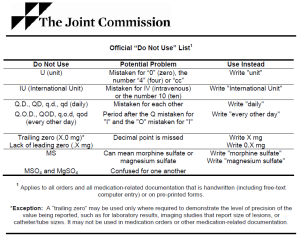
In 2001, The Joint Commission on Accreditation of Healthcare Organizations approved a National Patient Safety Goal requiring accredited organizations to implement a list of abbreviations not to use. In 2004 they introduced their “Do Not Use” list of abbreviations including “U” for units, “IU” for international units, “QD” or “QOD” for daily or every other day, “X.0 mg” or “.X mg” for fear of missed decimal points, or “MS” for confusion between morphine sulfate and magnesium sulfate [5]. However, this requirement does not apply to preprogrammed health information technology, and abbreviations remain common in electronic medical records. Advancements in electronic medical records, including electronic prescription use, can help, but free-text to describe medications and typed patient histories are not affected by these systems. Not only do these abbreviations make it difficult for individuals to fully understand a patient’s history and prescribe the correct medication, but abbreviations in progress notes and discharge summaries also hinder the ability to extract meaningful data for retrospective analyses [6].
To rectify these problems, a study done in an emergency room at a tertiary care center developed an unapproved abbreviations list and, using a computerized tool to detect the unapproved abbreviations, provided doctors with individual feedback at the end of each month on their abbreviation use with comparisons to peers. After six months, they found a 29% decrease in abbreviation usage [7]. While not perfect, this system of individualized feedback and “shaming” by comparison is an option for encouraging a move away from the dangerous and easily avoidable practice of ambiguous abbreviations.
Benjamin Rodwin is a 3rd year medical student at NYU School of Medicine
Peer reviewed by Michael Tanner, MD, Associate Editor, Clinical Correlations
References:
1. Brunetti L, Santell JP, Hicks RW. The impact of abbreviations on patient safety. Jt Comm J Qual Patient Saf. 2007:33(9):576-583. http://www.ncbi.nlm.nih.gov/pubmed/17915532
2. Sheppard JE, Weidner LC, Zakai S, Fountain-Polley S, Williams J. Ambiguous abbreviations: an audit of abbreviations in paediatric note keeping. Arch Dis Child. 2008:93(3):204-206. http://www.ncbi.nlm.nih.gov/pubmed/17986605
3. Sinha S, McDermott F, Srinivas G, Houghton PW. Use of abbreviations by healthcare professionals: what is the way forward? Postgrad Med J. 2011:87(1029):450-452. http://www.ncbi.nlm.nih.gov/pubmed/21459778
4. Dooley MJ, Wiseman M, Gu G. Prevalence of error-prone abbreviations used in medication prescribing for hospitalised patients: multi-hospital evaluation. Intern Med J. 2012;42(3):e19-e22. http://www.ncbi.nlm.nih.gov/pubmed/22432997
5. The Joint Commission. Facts about the official “Do Not Use” list of abbreviations. http://www.jointcommission.org/about_us/patient_safety_fact_sheets.aspx. Updated June 28, 2012. Accessed August 16, 2012.
6. Wong W, Glance D. Statistical semantic and clinician confidence analysis for correcting abbreviations and spelling errors in clinical progress notes. Artif Intell Med. 2011:53(3):171-180. http://www.ncbi.nlm.nih.gov/pubmed/21924593
7. Capraro A, Stack A, Harper MB, Kimia A. Detecting unapproved abbreviation in the electronic medical record. Jt Comm J Qual Patient Saf. 2012:38(4):178-183. http://www.ncbi.nlm.nih.gov/pubmed/22533130