Podcast: Play in new window | Download
Subscribe: RSS
By Shira Sachs MD, Stephanie Sherman MD, Cindy Fang MD and John Hwang MD || Audio Editing by Richard Chen || Graphic by Amy Ou MDTime Stamps
- Player three has entered the game! [0:15]
- Case presentation, part 1 [1:20]
- First impressions [3:24]
- Rethinking another provider’s diagnosis [4:36]
- Interpreting the test of treatment [9:42]
- Keeping your instincts on a leash? [10:58]
- Case presentation, part 2 [12:33]
- Diagnostic schemas [14:30]
- Our discussant’s differential and the final diagnosis [17:46]
- Shira’s cognitive autopsy [23:02]
Show Notes
- “Diagnostic momentum” refers to our conscious or unconscious tendency to avoid rethinking a diagnosis that has already been “assigned” to a patient.
- While most diagnoses made by doctors are correct, many are not.
- Since it is often impractical to comprehensively question every assigned diagnosis, learning to recognize when these labels do not fit the patient is an essential skill.
- The test of treatment is a legitimate diagnostic tool, but like any test, it can produce false positive and false negative results.
- False positive: A doctor may misdiagnose angina if her patient’s chest pain improves with nitroglycerin, when in fact it remitted spontaneously.
- False negative: A patient with obstructive sleep apnea may complain of persistent symptoms despite positive airway pressure, when in fact the prescribed settings may simply be insufficient.
- The term “diagnostic schema” describes a clinician’s structured approach to a recurring clinical problem.
- Experts have robust schema for problems within their discipline, which enable them to dissect cases featuring these problems efficiently and accurately.
- Extensive reading and deliberate clinical practice are needed to refine the schema we “inherit” from our medical training as novices (e.g. “pre-renal, intrinsic, and post-renal causes of acute kidney injury).
- The cognitive autopsy is a self-reflection exercise in which the clinician retrospectively interrogates their thought process to identify cognitive errors and areas for improvement in their reasoning.
Transcript
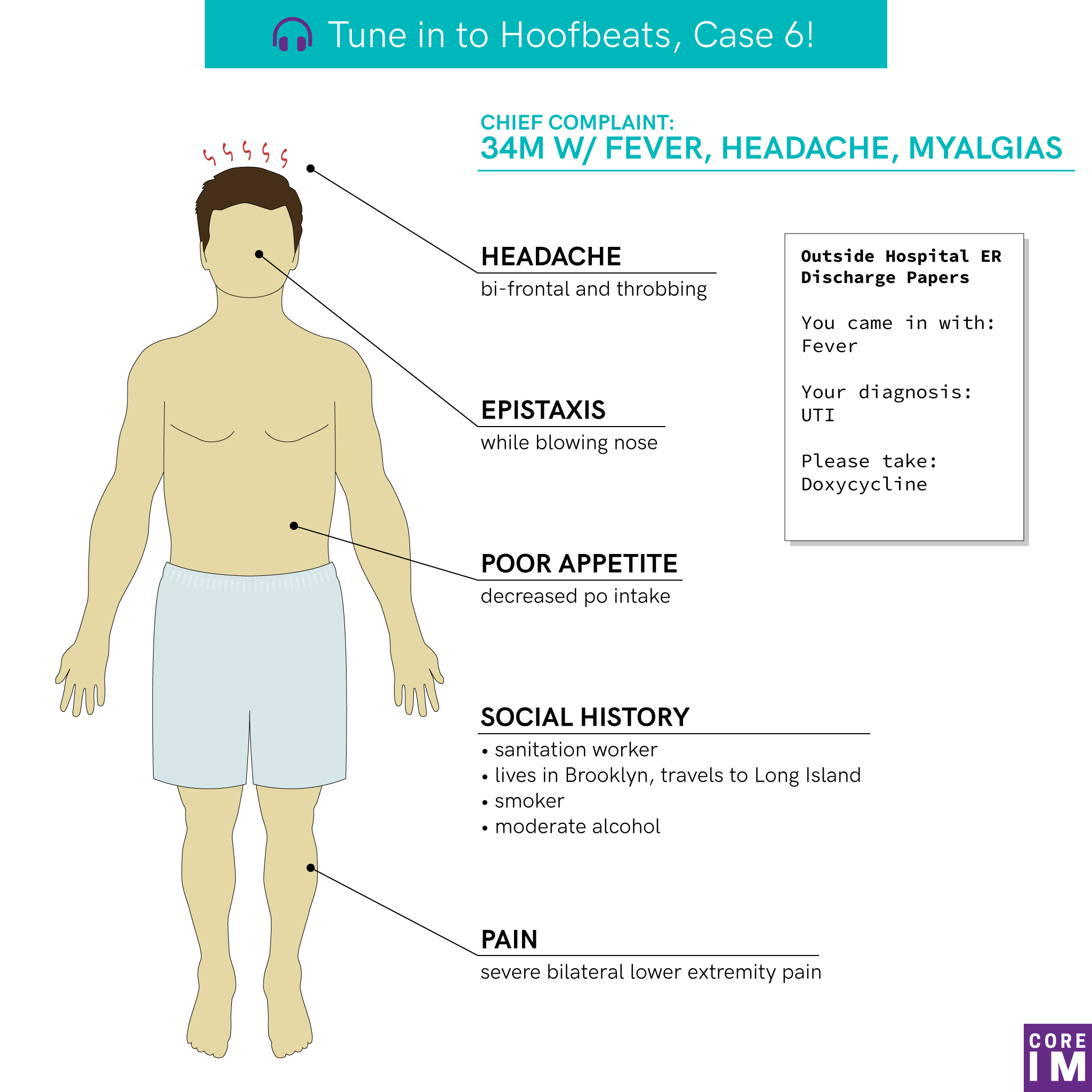
CINDY Hey everyone, Cindy Fang here. Thanks for tuning in. And we have something new for you this month. JOHN Someone new, rather. Hoofbeats listeners: meet Dr. Shira Sachs. SHIRA What’s up, guys? JOHN So, Shira, welcome — it’s so great to have you. Can we have you tell our listeners a bit about yourself? SHIRA For sure, it’s great to be here. So I recently moved here from Houston, Texas, where I did my residency and a chief year, after which I worked as a hospitalist for a year down at Baylor, and I just moved to New York in July and have been a hospitalist at Cornell since then, as a part of the hospital medicine fellowship medicine program there, the clinical scholars program. JOHN Well, it’s a real privilege to have you here. CINDY And Shira came to us with a case that we think you’ll really enjoy. SHIRA Yeah, today we’re going to reason through a great case I saw on wards with my team a few months ago. It’s an interesting multisystem disease process, and I really hope you guys enjoy solving it as much as I did. CINDY And before Shira gets started, I’d like to say thank you to all our listeners for all your support. Now we’re going to pass the mic to Shira and announce our early retirement. CASE PRESENTATION JOHN Yep. As part of our exit clause, I’m going to present Shira’s case. Then you’re in her capable hands. So, Shira’s patient is a previously healthy 34-year-old man presenting with resolved fever and ten days of headache and myalgias. The story he tells is that, ten days ago, he experienced 24-hours of subjective fever and chills. Subsequently, he develops severe pain in his bilateral lower extremities, particularly in his calves, without any weakness or parasthesias. He also experiences a bi-frontal, throbbing headache over this time period, without any photophobia, nausea, or vomiting. He feels generally fatigued with a poor appetite and decreased PO intake. He takes ibuprofen 600mg every six hours and gabapentin 300mg nightly, but these don’t bring him any relief. Three days after his symptoms begin, he presents to an outside ER where he is diagnosed with a UTI and prescribed doxycycline. But he discontinues this after four days as his symptoms remained unchanged. Of note, the patient denied any dysuria, urgency, abdominal pain, or flank pain at the time of this diagnosis. Two days later, he has an episode of epistaxis while blowing his nose and presents to the same outside ER for evaluation. At that point, he is found to have multiple lab abnormalities, prompting his transfer to for further care. The patient is a sanitation worker in NYC. He stays in an apartment in Brooklyn during the week and travels to Long Island on the weekends to be with his wife and children. He denies any travel outside of NY. He smokes one pack per day and drinks a 6-pack of beer on weekends. Shira Based on the history so far, take a few minutes to organize your thoughts and we’ll meet back up after the break! ♫ Musical Interlude ♫ Shira Welcome back! I sat down with my friend and mentor Dr. Stephanie Sherman, an academic hospitalist at Baylor College of Medicine in Houston, Texas. Let’s hear her initial approach to the case. SHERMAN Really in the first bit of the story, we see that we have a healthy young adult who’s got an acute febrile illness. And in that host, my first concern immediately was an infectious etiology. Knowing though that there’s many other categories that can give an acute febrile illness, I think it is important early on to remain open to autoimmunity, malignancy, and also endocrinopathies, or systemic drug reactions SHERMAN The specific symptoms accompanying his fever, the headaches, myalgias, fatigue, anorexia, really seemed pretty nonspecific at this point, could fit with a lot of different acute viral or bacterial conditions Shira Ok so far, we have a healthy guy with an acute febrile illness and relatively non-specific symptoms, overall this picture is most concerning for an underlying infection. Dr. Stephanie Sherman quickly turned to the patient’s prior contacts with the health care system to provide more rich and really diagnostically useful information. STEPHANIE SHERMAN And my general approach, when I’m not the first clinician to see someone and when I have data of what those clinicians thought in their earlier evaluations, is that it’s really honestly incredibly important to step back and not necessarily use the clinicians’ interpretations of what was going on, but consider really what primary data they collected to make them come to those decisions. Specifically when he went to the outside ER about a week before getting hospitalized, they diagnosed him with a UTI. This was surprising, because we find out he doesn’t have any dysuria, any flank pain, any overt hematuria. And so I wondered is what the ER physicians actually saw a UA that had white cells and red blood cells on it. So I think thinking broadly about this positive UA and considering well, what reasons could there be for there to be cells in his urine besides a standard UTI was an important clue early on in the case. Sterile pyuria, meaning white cells in the urine without a typical positive urine culture, can happen in a lot of different situations. But it also made me think early about processes that could give him white cells in the urine from interstitial nephritis, from allergic triggers, perhaps like the NSAIDs he’s taking, autoimmune conditions that may unfold, like sarcoid, or other infections that directly infect the interstitium: CMV, Legionella, leptospirosis fall in those categories. Shira I think Dr. Stephanie Sherman’s approach here is really worth reviewing. Our patients have often seen multiple providers before we meet them, and we need to be keenly aware of when a diagnostic label just doesn’t make sense. For instance, when Dr. Stephanie Sherman hears about the presumptive UTI diagnosis in the absence of any symptoms, her spidey senses immediately go off and she starts thinking about other reasons why the patient may have had pyuria. She quickly hones in on a few discrete infections that could both explain the patient’s non-specific symptoms, and potentially involve the kidney through interstitial nephritis. This is so important as the failure to set aside an incorrect diagnostic label can lead to the bias of diagnostic momentum, in which we accept a diagnosis without re-evaluating the data for ourselves. This only further propagates misdiagnosis and creates delays in care. With repeated exposure to a particular chief complaint or set of symptoms, our sense of when a diagnostic label doesn’t fit becomes further refined, as Dr. Stephanie Sherman exemplified in her interpretation of the patient’s prior UTI diagnosis. ♫ Brief music pause ♫ STEPHANIE SHERMAN The other really interesting thing we get from his interaction with the healthcare system before the hospitalization is his treatment with doxycycline. This stood out to me for a couple reasons. One is it’s a curious choice for a UTI. It doesn’t quite fit the standard organisms we’d expect for him. And in practice, I feel like we often reach for doxy in more mysterious febrile illnesses, treating so called “doxy-deficient conditions”. Really, meaning, were the clinicians worried about a zoonotic or rickettsial infection early on? Shira Actually, on review of his records, the peculiar choice in antibiotic was intended to treat for possible Chlamydia urethritis. Interestingly though, Dr. Stephanie Sherman uses this data point to consider whether they too were worried about certain “doxy-deficient conditions” that may already be on her differential. Were you considering any particular zoonotic or Rickettsial infections? If so, what do you think about his response to an empiric trial of doxy? Let’s hear Dr. Stephanie Sherman’s take… STEPHANIE SHERMAN The other interesting thing about the doxy is he didn’t feel better on it. And when trying to diagnose a case in a patient who has interacted with other healthcare providers earlier, how they respond to a treatment can give us some helpful diagnostic information. In this case, I wondered, did he not feel better because the doxy wasn’t appropriate, or was it not quite strong enough for what he had? Or, I did wonder perhaps the medication itself did help, but his underlying condition flared in the setting of systemic therapy. And the particular thing to watch out for would be the systemic inflammatory response from antibiotics in spirochete-induced diseases, the Jarisch-Herxheimer reaction. So his lack of response to the antibiotic I think could be interpreted in a lot of different ways. It still keeps our differential diagnosis pretty broad, but it does give us a little more information knowing how he did or did not respond to treatment. Shira Here, Dr. Stephanie Sherman is using what’s called the test of treatment by gauging the patient’s response to a trial of doxycycline. In reality, we use the test of treatment all the time. For instance, have you ever started PPI’s empirically for symptoms that sounded like GERD? As with any diagnostic test though, there are important scenarios in which the test of treatment can yield either false positive or false negative results. A false positive can occur if the underlying disease process just spontaneously resolves. False negative results can occur if the treatment dose or duration are inadequate. Ideally, if you were concerned for a “doxy-deficient condition” you could identify objective parameters to follow over time to help confirm whether you reached the right diagnosis. What do you think happened in this case? What would you monitor in this patient if you decided to start a trial of doxy? ♫ Brief music pause ♫ Shira let’s get back to our case and hear Dr. Stephanie Sherman’s thoughts on the social history. STEPHANIE SHERMAN The social history, social history as expected was very helpful. I immediately saw his occupation and had a tendency to sort of start to anchor on the fact that as a sanitation worker he has human and animal waste exposures. Leptospirosis fits into the illness script of that with exposure, particularly to rodent excrement and urine. But just because he works in sanitation doesn’t mean he can’t have any other disease. So I sort of quickly stepped in that direction, and stepped away. Shira Dr. Stephanie Sherman is taking a cautious approach to the patient’s exposure history. It’s an important data point, and if we treat it like a diagnostic test it certainly increases her post-test probability of Lepto. However that doesn’t mean the probability of other diagnoses on her differential have become so low that’s it’s not worth investigating these other possibilities. If I were in Dr. Stephanie Sherman’s place – I can easily imagine myself getting over-excited about having potentially identified a zebra that could explain all my patient’s symptoms. However, it’s important to set aside these types of emotional responses, and really consider – based on what I know right now – can I really say the probability of other diagnoses on my list has now become zero? Dr. Stephanie Sherman is avoiding anchoring bias by keeping in mind that many other diagnoses remain plausible at this point and are worthy of further workup, despite this intriguing morsel of data. ♫ Brief music pause ♫ Shira At this point, let’s get to the physical exam and admission labs. CASE PRESENTATION JOHN On presentation to NYP, the patient was afebrile and hemodynamically stable. He was athletic appearing. He had scleral and sublingual icterus with diffuse jaundice. There were scattered petechiae on the chest and back without any other visible rashes or lesions. There were no oropharyngeal lesions or cervical LAD. Heart and lung exam were unremarkable. His abdomen was soft and non-tender without any appreciable hepatosplenomegaly. Lower extremity strength, sensation, and reflexes were all within normal limits. CBC was notable for a WBC of 19,200 with 58% neutrophils and 5% bands, a Hgb of 12.4, and a Plt count of 62,000. BMP revealed a K of 3.3 and BUN/Cr of 73/1.6, respectively. LFTs were notable for total bilirubin of 21.2, direct bilirubin of 16.8, AST of 70, ALT of 45, and AP of 132, with a GGT of 208. Shira Let’s go ahead and take a break here. Consider pausing the episode and re-evaluating your differential based on this new information before we hear Dr. Stephanie Sherman’s thoughts. ♫ Musical Interlude ♫ Shira Welcome back guys. So just to review, we’re trying to solve this case of a 34 year old man who looks like he has an acute, febrile, multisystem illness. What did you think was going on? Here’s our discussant’s reaction to what you just heard. STEPHANIE SHERMAN Some of the labs were not surprising and some were very surprising, and I think this was a pretty critical pivot point in the case. So for example, the leukocytosis right now is not surprising. It speaks to the systemic inflammation he’s going through. The thrombocytopenia similarly could go with the infectious hypothesis. If it’s from sepsis directly, the infection itself affecting the bone marrow, or a consumptive process like DIC or a thrombotic microangiopathy. The kidney injury, in some ways isn’t surprising given some of the hits that he’s taken. The ibuprofen around the clock, the limited oral intake. But again, we do have a presumed pyuric UA from the prior hospital stay, so more intrinsic renal injuries are possible as well to his prerenal state. Finally though, the liver biochemical tests were really the twist and the big surprise. When encountering liver tests in general, I stick to the approach of categorizing the pattern of the abnormality first, and then building the differential for those abnormalities from there. So out of a hepatocellular versus cholestatic versus infiltrative pattern, which would be mostly AST/ALT elevations versus mostly bili and alk phos elevations versus mostly in isolated alk phos, respectively, he just has a very clear cholestatic pattern driven by his hyperbilirubinemia with associated alk phos as well. The key approach here will be later on with diagnostics figuring out is this from biliary obstruction, either within or outside the liver, or is there more of a cholestatic liver injury itself? But this was very surprising and I think makes us kind of go back to that original list and broaden things and consider infections that really have more of a direct liver effect as well. Shira In thinking about the patient’s labs, Dr. Stephanie Sherman is applying her diagnostic schema for abnormal LFT’s. Diagnostic schemas are cognitive tools that provide a scaffold from which to break down more complex clinical problems. For instance, when you heard thrombocytopenia, did you immediately start sub-categorizing diagnoses by decreased production, increased destruction, and sequestration? That’s an example of a commonly used diagnostic schema you’ve likely heard in the past. Why is this useful? Well it allows you to retrieve from memory well organized lists of potential diagnoses to consider. They’re also handy as a tool for thinking-out-loud to teach your clinical reasoning to others. We all start to develop diagnostic schemas early in training and refine them over time with repeated exposure to similar clinical scenarios. Here Dr. Stephanie Sherman is quickly able to focus in on a cholestatic pattern, leading her to consider obstruction pathologies vs. processes that cause direct injury to the bile ducts. Shira Alright team, pause here and refine your problem representation before we hear Dr. Stephanie Sherman’s version. ♫ Brief music pause ♫ STEPHANIE SHERMAN With all of that said, we are treating a healthy young sanitation worker with an acute onset febrile syndrome with headaches, myalgias, cholestatic liver injury, thrombocytopenia, and an AKI with microscopic hematuria. So really a multiorgan inflammatory state, in which the clinical scenario still seems most compelling and most pressing to look for infection. And I would go back to the infection category being broken down even more thoroughly by bacteria, viral, etc, and sort of force myself at this point to commit to what organisms I’m most worried about. Shira What do you think of Dr. Stephanie Sherman’s problem representation? How did it compare to what you came up with? Consider pausing again here to put the finishing touches on your differential diagnosis before we get to Dr. Stephanie Sherman’s final thoughts on the case. STEPHANIE SHERMAN In the bacterial category I think abscesses or bacteremia from staph, strep at this point are possible. We’d really have to explain why the liver is getting hit so hard. But then as well as gram-negative infections with severe sepsis. Salmonella potentially could be an explanation as well, although the bilis are probably little too high to be explained by pure systemic sepsis alone. I still do worry about actual involvement of the liver. Viral, you know, I think viral hepatitis, my illness script really includes much more dramatic hepatocellular AST/ALT elevations. But, I’d want to keep those on the table given how much hepatobiliary injury there is. I think flu, epstein barr virus, CMV, and of course checking for HIV, both as a primary driver of this, but to inform his immune status is important. Finally, I think finishing with the category of atypical or specifically spirochete or rickettsial organisms, this is definitely important given what we found in the social history. So thinking about, disseminated syphilis is a possibility, perhaps scrub typhus. As far as I know, in New York murine typhus really isn’t as a problem, but here in Houston where I practice that would definitely be on the table for this serious illness. And then again with the potential animal waste exposure, leptospirosis could tie this all well together. It would have to be the very kind of severe syndrome of Weil’s disease. Noninfectious again, is still on there. The endocrinopathies could be possible, very severe thyrotoxicosis, adrenal insufficiency. And then in the autoimmune categories, I want to tie the hepatobiliary disease in well, so thinking about an unexpected presentation of sclerosing cholangitis, autoimmune hepatitis. But again, the time course, the fact the AST and ALT aren’t that high, just don’t fit very well. Shira I really like how Dr. Stephanie Sherman organized her differential. She had honed in on infection early, but broke down discrete diagnoses further by bacterial, viral, and atypical infectious categories. Finally she made sure to include non-infectious processes that could still be at play here. Instead of just listing off discrete diagnoses, sub-categorizing by microbiological class allowed her to be very systematic and comprehensive in how she approached the case. Consider pausing and writing down what additional workup you would order at this point, before we reveal what happened next. ♫ Fade into medium music pause ♫ Shira Ultimately, blood and urine cultures remained without growth. HIV antibody testing and viral load were both negative. HAV, HBV, and HEV serologies were non-revealing. Serologies for EBV and CMV revealed negative IgM’s with positive IgG’s consistent with prior exposure, with negative VL’s for both organisms. Lyme serologies were negative. Anaplasma/Ehrlichia smear was negative as were Anaplasma serologies. Abdominal US and MRCP were both negative for intra or extrahepatic biliary dilation, though MRCP did show prominent abdominal and retroperitoneal lymphadenopathy. The patient was empirically restarted on doxycycline given the high clinical suspicion for Leptospirosis. His leukocytosis, thrombocytopenia, AKI, and hyperbilirubinemia all improved on doxycycline, and ultimately Leptospirosis IgM returned positive after the patient had already been discharged from the hospital. ♫ Brief music pause — a few seconds ♫ Shira When I evaluated this patient for the first time, my problem representation included a previously healthy young man who worked in sanitation with resolved fever, presenting with headache, and myalgias, and prominent lab abnormalities including leukocytosis, thrombocytopenia, AKI, and profound hyperbilirubinemia. I was considering Anaplasma/Ehrlichia, EBV, CMV, and Rickettsial infections. But what really didn’t fit for me was the extremely high Tbili which just didn’t match with my illness scripts for these diagnoses. Lepto was just not on my radar, but I had a feeling there was something that I was missing. After a few hours of independent reading, I walked next door to run the case by some colleagues, who brought up the possibility of Leptospirosis. Notably, I later learned Lepto actually migrates between hepatocytes, detaching intercellular junctions, and disrupting bile canaliculi, which can cause the degree of hyperbilirubinemia that was seen in this case. I asked Dr. Stephanie Sherman how she deals with similar diagnostic dilemmas. STEPHANIE SHERMAN Um, but honestly there’s, that’s the fun of medicine is we just, we won’t see things a lot of the time. Weil’s syndrome in particular, I’ll say I’ve never seen it. Maybe our rats are cleaner here in Houston. And actually this is something I have seen presented as conferences as kind of a, just a diagnostic challenge. So that’s how I think getting exposure, even when you don’t see cases clinically, it’s just listening to cases, talking with colleagues and reading. But back to the reality of being in the moment, feeling like you’re missing something, I think sort of zooming out and coming up with the most kind of condensed problem list as possible, and then just using the resources you have to see what hits come up for those combinations. Shira I think Dr. Stephanie Sherman’s on the right track. In performing a cognitive autopsy, to better understand how my own cognitive errors played a role in the case, I should have reached out for help earlier. I think as clinicians, we can feel all this pressure to have the answers in every clinical scenario. This is just unrealistic given the complexity of medical care we face today. Our colleagues are an amazing resource that in this case led me the ultimate diagnosis. I also probably underutilize the simple Google search. In preparing for this episode I entered my problem representation in Dr. Google, and low and behold Leptospirosis is the first thing that comes up! So, for me – letting go of the expectation that I can figure it all out myself, and utilizing the ample resources around me were some important takeaways. Take-home points and conclusion. Shira Let’s summarize our take-home points for today. When working up a patient who has had prior contact with the health care system, be attuned to when diagnostic labels don’t fit and require re-evaluation to avoid the bias of diagnostic momentum. Recognize when you are using the test of treatment as a diagnostic test, and understand that both false positive and false negative results can occur in the situations we discussed earlier in the episode. Be deliberate about developing, refining, and teaching your diagnostic schemas, they can save us a lot of mental energy in the clinically complex setting in which we practice medicine. Finally, after having some time to decompress after a challenging or difficult case, think about doing a cognitive autopsy to crystalize how you would change your approach next time around. Shira That’s all for now folks! I want to thank our guest, Dr. Stephanie Stephanie Sherman. Thank you to Drs. Shreya Trivedi, John Hwang, and Cindy Fang for weighing in this episode, along with Michael Shen, Amy Ou, and our audio editors Richard Chen and Harit Shah. As always, an honorable mention to our fellow podcaster Dr. Steven Liu. CINDY And Hoofbeats listeners, in case it needs to be said — John and I aren’t actually retiring. We’ll be back next episode. JOHN Of course. Truth is, we like doing this too much! But we just know there are more Shiras out there among you. Brimming with cases, ideas, probably with a completely different perspective on how to think, or teach, or learn about clinical reasoning! Well, we would love to hear your thoughts. Send us an email at CoreIMpodcast@gmail.com. We are also on facebook, and twitter, at @CoreIMpodcast. CINDY Opinions expressed in this podcast are our own, and do not represent the opinions of WCM or other affiliated institutions, nor should they be construed as medical advice. With Core IM, I’m Cindy Fang… JOHN I’m John Hwang. SHIRA And I’m Shira Sachs. I’ll see you guys next time!References
- Croskerry P. Diagnostic Failure: A Cognitive and Affective Approach. In: Henriksen K, Battles JB, Marks ES, et al., editors. Advances in Patient Safety: From Research to Implementation (Volume 2: Concepts and Methodology). Rockville (MD): Agency for Healthcare Research and Quality (US); 2005 Feb. Available from: https://www.ncbi.nlm.nih.gov/books/NBK20487/
- Glasziou, P., Rose, P., Heneghan, C., & Balla, J. (2009). Diagnosis using” test of treatment”. BMJ: British Medical Journal (Online), 338.
- Kassirer JP, Wong JB, Kopelman RI. Learning clinical reasoning. Baltimore, MD: Wolters Kluwer/Lippincott Williams & Wilkins; 2010

4 comments on “Core IM Hoofbeats: 34M with Fever, Headache and Myalgias”
Another excellent episode. One of the characteristic symptom of leptospirosis taught during my med school is tenderness in the calf region and that is one of the clue that anchored me towards the diagnosis, though I do wonder whether it is really specific.
I work in ED and its very unlikely I start a patient on doxy for uti . I wonder what was the UA report what triggered the provider to choose doxy is there anything we are missing on HPI .
Suffice to say ; best case ever thank you all especially your cognition autopsy great vignettes .
This case underlines the importance of “occupational or travel” history in a patient presenting with fever with rash or blisters. Very good discussion about differential. Thanks.
No joke, not two days after listening to this episode I admitted a 42yo male with 1 week of headache, myalgias, and fever. He came in septic with no obvious source. He is a hunter who has multiple potential Rickettsial and zoonotic exposures, but he is also a sewer worker! Of course I had to check, and lo and behold his leptospiral IgM antibody popped up positive yesterday. He was much improved after just a day of doxycycline. Crazy coincidences aside, I really enjoy these Hoofbeats episodes. I find myself more formally examining my diagnostic reasoning and I have developed a more structured approach to teach my residents how to improve theirs. Keep up the good work!
Comments are closed.