Peer Reviewed
Introduction
QT interval prolongation is a common side effect shared among the most effective antiemetic classes. The risk of QT prolongation is exacerbated by electrolyte abnormalities observed in patients with ongoing emesis, particularly hypokalemia. While QT prolongation in itself is not harmful, it increases the risk for developing a polymorphic ventricular arrhythmia aptly named torsades de pointes (TdP), French for “twisting of the points”, because of its appearance of a twisting ribbon around the electrocardiogram (ECG) baseline. TdP can rapidly degenerate into ventricular fibrillation and cardiac arrest.
Antiemetics Causing QTc Prolongation
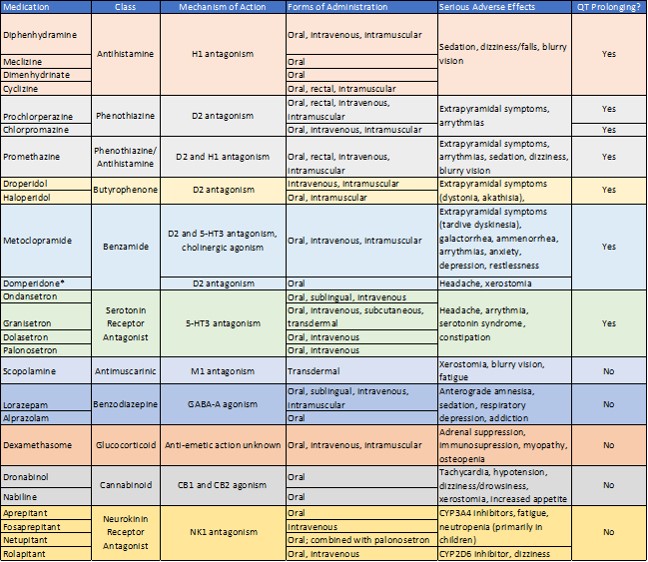
Numerous antiemetics are available to practitioners and differ in both the receptors they target and side effect profiles. Table 1 presents a list of commonly used antiemetics, their class, mechanism of action, side effects, and effect on the QT interval.
Antihistamines are used primarily in the management of pruritus and allergic reactions. However, they can also be used to treat motion sickness-associated nausea. The antiemetic effect is via H1-histamine receptor antagonism within the area postrema (1). The use of antihistamines is limited by anticholinergic side effects including sedation, dizziness, and blurry vision. The mechanism by which antihistamines prolong QTc is inhibition of the delayed rectifier potassium current (IKr), a potassium efflux channel, resulting in prolonged cardiomyocyte repolarization (2).
Phenothiazines, butyrophenones, and benzamides are all antiemetic classes that function primarily by inhibiting dopamine receptors within the area postrema. Although they provide powerful symptom relief, their use is limited by both extrapyramidal side effects and QTc prolongation. Metoclopramide is a commonly used benzamide, which crosses the blood-brain barrier and inhibits dopamine receptors within the basal ganglia. Due to dopamine blockade, adverse reactions include dystonia, akathisia, and tardive dyskinesia (3). Although dystonia can be relieved with the administration of antihistamines, tardive dyskinesia is a permanent and disabling side effect. Metoclopramide carries a black box warning from the FDA regarding the risk of tardive dyskinesia with long-term use (4). To address the side-effects of metoclopramide, domperidone was developed as a peripherally-acting dopamine antagonist that is unable to cross the blood-brain barrier. However, its use is restricted and requires special approval via the FDA investigational drug protocol. The exact mechanism by which benzamides induce QTc prolongation is uncertain, but recent studies suggest they block cardiac voltage-gated sodium channels, which may serve to explain some of their cardiotoxic effects (5). Both phenothiazines and butyrophenones are known to cause QTc prolongation because of their inhibition of IKr potassium efflux channels and are similarly limited by extrapyramidal side effects (2, 6). Newer generations of butyrophenones, such as olanzapine, have demonstrated lower risks of cardiotoxicity and extrapyramidal side effects, however, their degree of antiemetic efficacy remains to be elucidated.
The final category of QTc-prolonging antiemetics is the serotonin receptor antagonists. These include ondansetron and its derivatives; granisetron, dolasetron, and palonosetron. Serotonin receptor antagonists are considered the cornerstone of antiemetic management in patients undergoing chemotherapy (7). They are incredibly effective and do not have the extrapyramidal side effects seen with the dopamine receptor antagonists. Despite their relative safety, they also cause QT prolongation. Similar to other QT-prolonging antiemetic classes, serotonin receptor antagonists cause QTc prolongation by inhibiting the IKr potassium efflux channels, thus prolonging cardiac repolarization (8). Different forms of medication delivery may mitigate QTc-prolonging effects. Transdermal granisetron has been shown to have less effect on the QT interval than other medications within its class and is equally efficacious to its oral formulation (9).
Antiemetics That Do Not Cause QTc Prolongation
Hospitalized patients are at risk for acquired QTc prolongation in the setting of medication administration and electrolyte abnormalities. Therefore, clinicians should be familiar with antiemetic classes that can be safely used in patients who have an established prolonged QTc.
Scopolamine is an antimuscarinic mediation with a similar anticholinergic side effect profile as antihistamines. However, by acting as an M1-muscarinic antagonist, it is non-sedating and does not prolong the QTc. Its use is limited to motion sickness prophylaxis and it is only available as a transdermal patch (10).
Benzodiazepines, specifically lorazepam and alprazolam, can be used to treat acute nausea in the inpatient setting. However, the degree of symptom relief is minimal, and their use is limited by sedation, anterograde amnesia, concerns for addiction, and risk of delirium in the elderly (11, 12). Their effect as an antiemetic is more likely related to anxiolysis and mitigation of anticipatory emesis rather than a direct effect on the area postrema (13).
Glucocorticoids, particularly dexamethasone, has well-established antiemetic properties and is used to treat chemotherapy-induced vomiting (14). The mechanism by which glucocorticoids treat nausea and vomiting is unclear. Furthermore, their use is limited by numerous adverse effects including adrenal suppression, infection, hyperglycemia, myopathy, and osteopenia (15). The risks and benefits of glucocorticoid administration should be carefully weighed before being used to treat nausea and emesis in patients with a prolonged QTc.
Finally, newer antiemetic agents include cannabinoids and neurokinin receptor antagonists. The efficacy of cannabinoids as antiemetics is modest and their use is limited in older patients by the side effects of tachycardia, hypotension, and xerostomia (16). Additionally, their effect as appetite stimulants induces increased food intake, which subsequently may result in more nausea and vomiting. Neurokinin receptor antagonists have shown greater promise as antiemetics and act on neurokinin receptors within the area postrema. Although they do not cause QTc prolongation, they do inhibit the CYP3A4 system and are likely to interact with other medications (17). Furthermore, given that neurokinin receptor antagonists are a novel class of medications, their use is likely to be cost-prohibitive.
Conclusion
Numerous treatment options are available for the management of nausea and vomiting. Recognizing which antiemetics can be safely used and their side effect profiles is crucial for effective patient care.
Table 1 List of Commonly Used Antiemetics (18)
*Only available through the FDA’s investigational drug protocol
Dr. Ofer Fass is a chief resident, internal medicine, NYU Langone Health
Peer reviewed by John Papadopoulos, PharmD, Clinical Assistant Professor, Medicine, NYU Langone Health
Image courtesy of Wikimedia Commons
References
- Church MK. H(1)-antihistamines and inflammation. Clin Exp Allergy. 2001;31(9):1341-3.
- Nachimuthu S, Assar MD, Schussler JM. Drug-induced QT interval prolongation: mechanisms and clinical management. Ther Adv Drug Saf. 2012;3(5):241-53.
- Bateman DN, Rawlins MD, Simpson JM. Extrapyramidal reactions with metoclopramide. BMJ .1985;291(6500):930-2.
- Rao AS, Camilleri M. Review article: metoclopramide and tardive dyskinesia. Aliment Pharmacol Ther. 2010;31(1):11-9.
- Stoetzer C, Voelker M, Doll T, Heineke J, Wegner F, Leffler A. Cardiotoxic Antiemetics Metoclopramide and Domperidone Block Cardiac Voltage-Gated Na+ Channels. Anesth Analg. 2017;124(1):52-60.
- Glassman AH, Bigger JT, Jr. Antipsychotic drugs: prolonged QTc interval, torsade de pointes, and sudden death. Am J Psychiatry. 2001;158(11):1774-82.
- Kaizer L, Warr D, Hoskins P, Latreille J, Lofters W, Yau J, et al. Effect of schedule and maintenance on the antiemetic efficacy of ondansetron combined with dexamethasone in acute and delayed nausea and emesis in patients receiving moderately emetogenic chemotherapy: a phase III trial by the National Cancer Institute of Canada Clinical Trials Group. J Clin Oncol. 1994;12(5):1050-7.
- de Lorenzi FG, Bridal TR, Spinelli W. Block of the delayed rectifier current (IK) by the 5-HT3 antagonists ondansetron and granisetron in feline ventricular myocytes. Br J Pharmacol. 1994;113(2):527-35.
- Mason JW, Moon TE. Use and cardiovascular safety of transdermal and other granisetron preparations in cancer management. Cancer Manag Res. 2013;5:179+.
- Clissold SP, Heel RC. Transdermal hyoscine (Scopolamine). A preliminary review of its pharmacodynamic properties and therapeutic efficacy. Drugs. 1985;29(3):189-207.
- Scharf MB, Kales A, Bixler EO, Jacoby JA, Schweitzer PK. Lorazepam-efficacy, side effects, and rebound phenomena. Clin Pharmacol Ther. 1982;31(2):175-9.
- Tannenbaum C. Inappropriate benzodiazepine use in elderly patients and its reduction. J Psychiatr Neurosci : JPN. 2015;40(3):E27-E8.
- Kris MG, Gralla RJ, Clark RA, Tyson LB, Groshen S. Antiemetic control and prevention of side effects of anti-cancer therapy with lorazepam or diphenhydramine when used in combination with metoclopramide plus dexamethasone. A double-blind, randomized trial. Cancer. 1987;60(11):2816-22.
- Basch E, Prestrud AA, Hesketh PJ, Kris MG, Feyer PC, Somerfield MR, et al. Antiemetics: American Society of Clinical Oncology clinical practice guideline update. J Clin Oncol. 2011;29(31):4189-98.
- Navari RM, Aapro M. Antiemetic Prophylaxis for Chemotherapy-Induced Nausea and Vomiting. N Engl J Med. 2016;374(14):1356-67.
- Jordan K, Schmoll HJ, Aapro MS. Comparative activity of antiemetic drugs. Crit Rev Oncol Hemat 2007;61(2):162-75.
- Rapoport B, Smit T. Clinical pharmacology of neurokinin-1 receptor antagonists for the treatment of nausea and vomiting associated with chemotherapy. Exper Opin Drug Saf. 2017;16(6):697-710.
- Longstreth GF HP. Characteristics of antiemetic drugs. UpToDate. Waltham, MA: Wolters Kluwer; 2018.