Peer Reviewed
Diabetes, a condition broadly characterized by the inability to maintain glucose homeostasis,1 can be classified into two primary subtypes: type 1 and type 2. Type 1 and type 2 diabetes are estimated to affect roughly 1.5 million and 32 million Americans, respectively – 10% of the U.S. population. Type 1 diabetes is characterized by the autoimmune destruction of pancreatic beta cells, rendering all those with the condition insulin-dependent. Roughly one-third of type 1 diabetics utilize insulin pump technology; the remaining two thirds use a multiple daily injection (MDI) regimen.2 Type 2 diabetes is characterized by the body’s inability to effectively utilize insulin and by the progressive impairment of beta cell function. Fewer than 1% of people with type 2 diabetes use insulin pump technology.3
Insulin pumps come in a variety of shapes and sizes; all models, however, require the patient to attach the pump externally. Prevalent models include the more conventional tubed pumps, including the Medtronic MiniMed and Tandem T-Slim.4,5 Tubed pumps represent the majority of insulin delivery systems, delivering insulin via an externally visible tubing and catheter system. Newer models, including Insulet’s Omnipod, have done away with tubing, thereby creating a less conspicuous and arguably more user-friendly system. Clinicians and researchers have demonstrated the benefits of insulin pump technology in insulin-dependent diabetes, and insulin pumps are nearly universally covered for this patient population. Copays and deductibles vary widely depending on insurance coverage, such that a patient’s out-of-pocket expenses for the pump and associated maintenance supplies (infusion sets, pods, etc.) must be individually computed and assessed.
Early innovations in diabetes research and device design focused on the prevention of hypoglycemia, which is more acutely dangerous than hyperglycemia.6-8 This manifested in the introduction of low-glucose insulin-suspend features. Through the integration of continuous glucose monitors (CGM) and automated pump systems, CGMs were programmed to send the glucose data they gathered directly to the insulin pumps to which they were paired. Insulin pumps then interpreted those data and automatically suspended basal insulin delivery, to the extent glucose levels were below a predetermined threshold.9
Subsequent trials built on this technology, incorporating what became known as the predictive low-glucose suspend (PLGS) feature.10-13 Whereas first-generation continuous glucose monitors were designed to capture and communicate real-time glucose data, second-generation monitors went one step further, incorporating an underlying algorithm to identify trends in glucose levels. Trends were used to predict whether a patient’s glucose was stable, trending up, or trending down, notifying the patient of a predicted low or urgent low to follow. Subsequent trials and devices used predictive data to preemptively suspend or lower basal insulin delivery in instances of an impending hypoglycemic event.14,15 Evidence gathered from several randomized controlled trials comparing PLGS to sensor-augmented pump therapy (SAP) pointed to statistically significant reductions in hypoglycemic events with the PLGS pump.16
Acknowledging the importance of maintaining broad-based glycemic control, a group of investigators turned their attention to the establishment of a more advanced “closed-loop” artificial pancreas system. Closed-loop systems are systems in which an insulin pump autonomously adjusts insulin delivery based on input from a paired CGM, establishing a “closed-loop” between blood glucose measurement and insulin delivery. Via this system, an algorithm targeting a pre-established and adjustable blood glucose target makes minor changes to the amount of insulin delivered based on the disparity between predicted blood glucose levels and the established target. In contrast with PLGS systems, closed-loop systems deliver micro-boluses in the setting of anticipated hyperglycemia as well as reduce or suspend insulin delivery in the setting of anticipated hypoglycemia. By extension, closed-loop systems aim to both improve time in range and prevent hypoglycemic events. The target range is estimated by serial hemoglobin HbA1c levels and is most commonly 70-180 mg/dl.
To date, over ten studies17-23 have investigated the effect of single-hormone closed-loop systems (also known as “artificial beta cell”20) on glycemic control; five others have investigated the effect of dual-hormone (insulin and glucagon) systems, on the same endpoint.24-27 Single-hormone studies have, on the whole, demonstrated statistically significant improvements in their preestablished primary endpoints, most often time in range. For example, a study of 585 adult and pediatric participants indicated that closed-loop systems increased time in range by 13 percentage points (p<0001).28 Another hybrid closed-loop study suggested that adults with a mean baseline HbA1c of 6.9% demonstrated further improvement in glycemic control while simultaneously reducing the burden of hypoglycemia.29 Dual-hormone systems have fared less well. Although the incorporation of glucagon facilitates the rapid fine-tuning of blood glucose levels and prevents hypoglycemia, researchers have been unable to synthetically produce a glucagon analogue that is chemically and physically stable enough for commercial use.30
The consistent demonstration of favorable outcomes achieved by closed-loop systems has paved the way for the commercialization of several single-hormone closed-loop artificial pancreas systems; Tandem Diabetes Care’s (San Diego, CA) Control IQ advanced hybrid closed-loop system was approved for use in 2020, whereas Insulet’s (Acton, MA) Horizon Automated Glucose Control System is currently under Phase III clinical trial investigation.31-32 While design and logistical limitations have, for the time being, prevented the commercialization of dual-hormone systems, researchers continue to investigate their commercial viability.
CGM and insulin pump technologies have tremendously altered the day-to-day lives of those living with diabetes. Having been diagnosed with type 1 diabetes at age 21, I vividly recall the minute puncture wounds to which my index finger was subjected six or seven times per day. As the number of finger sticks grew from the hundreds to thousands, these rapidly became confluent and noticeable to the naked eye and to my hyper-focused self. And what about the countless times my blood sugar monitor read 150 mg/dl, only to plummet to 55 mg/dl one hour later? Who was to predict the seemingly unpredictable blood sugar rollercoaster prior to the advent of the CGM?
The insulin pump was revolutionary for me. The days when I snuck my insulin pen beneath my desk and swiftly stabbed my thigh with insulin are over. What’s more, I could now enjoy the freedom of eating that “unplanned” cookie for dessert. A press of a button would allow for that, a decision previously relegated to a trip to the restroom. And these were the days before the closed loop system–the days when a fatty dinner could send my overnight blood sugars sky-high, inevitably setting me up for a hyperglycemic battle into the following morning. Having been fortunate to benefit from the closed-loop system for several months now, these occurrences occupy a significantly smaller part of my life.
CGM and insulin pump technologies are not without their limitations, however. These devices are…devices…that must be inserted into the subcutaneous tissue every 3-10 days. Depending on the manufacturer, the devices include tubing, a needle, catheter, and insertion set, which can be assembled and inserted within a few short minutes and with the press of a button (and a transient, albeit sharp prick). These devices also fail, leaving patients without insight into their blood sugar levels or, worse, without insulin until the failed device is replaced. And to add to your patients’ frustrations, they will inevitably spend yet another thirty minutes on the phone to replace that failed monitor or pump. Not to mention the countless calls placed to insurance companies, consistently requesting proof that your patient “still needs insulin” or “still benefits from pump therapy.”
Limitations and frustrations aside, these devices have forever changed the management of diabetes –not only proving to yield improvements in time in range and a reduction in hypoglycemic episodes, but also providing patients with a greater degree of autonomy and hope. Although researchers and clinicians have by no means provided our type 1 diabetic patients with new pancreases, they have immensely eased their burdens while trying.
Jessica Lovett is a 3rd year medical student at NYU Grossman School of Medicine
Reviewed by Michael Tanner, associate editor, Clinical Correlations
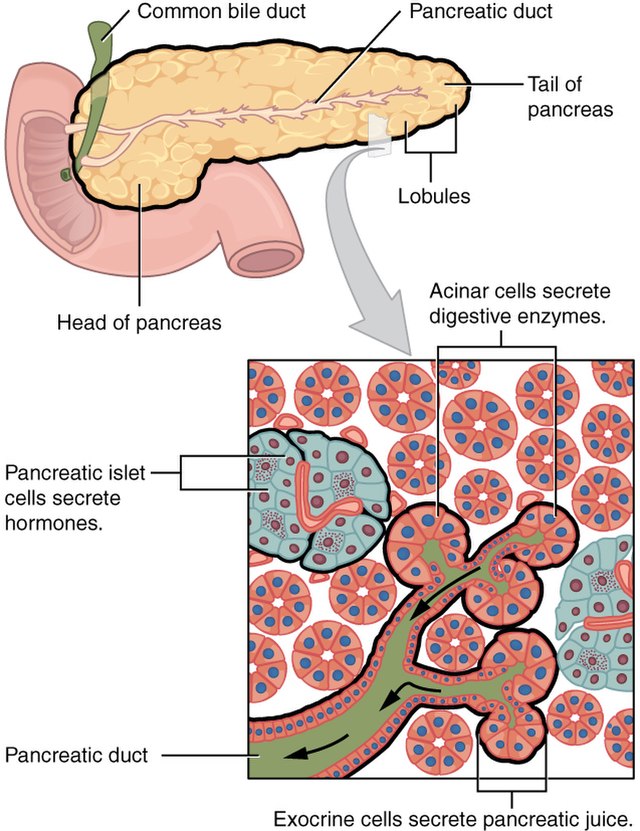
Image courtesy of Wikimedia Commons, source: 2424 Exocrine and Endocrine Pancreas.jpg, Author, OpenStax College
References
- American Diabetes Association. Classification and diagnosis of diabetes: Standards of medical care in diabetes 2021. Diabetes Care. 2021;44(Suppl. 1):S15-S33. https://care.diabetesjournals.org/content/44/Supplement_1/S15
- Corporation I. 10-K. In. Edgar, SEC2020.
- Umpierrez GE, Klonoff DC. Diabetes technology update: use of insulin pumps and continuous glucose monitoring in the hospital. Diabetes Care. 2018;41(8):1579-1589.
- Beato-Víbora PI, Gamero-Gallego F, Ambrojo-López A, Gil-Poch E, Martin-Romo I, Arroyo-Díez FJ. Rapid improvement in time in range after the implementation of an advanced hybrid closed-loop system in adolescents and adults with type 1 diabetes. Diabetes Technol Ther. 2021 April 21. doi: 10.1089/dia.2021.0037.
- Breton MD, Kovatchev BP. One year real-world use of control-IQ advanced hybrid closed-loop technology. Diabetes Technol Ther. 2021. 2021 Apr 21. doi: 10.1089/dia.2021.0097. https://pubmed.ncbi.nlm.nih.gov/33784196/
- Tauschmann M, Hovorka R. Technology in the management of type 1 diabetes mellitus – current status and future prospects. Nat Rev Endocrinol. 2018;14(8):464-475.
- Bergenstal RM, Klonoff DC, Garg SK, et al. ASPIRE In-Home Study Group. Threshold-based insulin-pump interruption for reduction of hypoglycemia. N Engl J Med. 2013;369(3):224-232.
- Ly TT, Nicholas JA, Retterath A, Lim EM, Davis EA, Jones TW. Effect of sensor-augmented insulin pump therapy and automated insulin suspension vs standard insulin pump therapy on hypoglycemia in patients with type 1 diabetes: a randomized clinical trial. JAMA. 2013;310(12):1240-1247.
- Bally L, Thabit H, Hovorka R. Glucose-responsive insulin delivery for type 1 diabetes: The artificial pancreas story. Int J Pharm. 2018;544(2):309-318.
- Pinsker JE, Bartee A, Katz ML, et al. Predictive low-glucose suspend necessitates less carbohydrate supplementation to rescue hypoglycemia: need to revisit current hypoglycemia treatment guidelines. Diabetes Technol Ther. 2021 Feb 18. doi: 10.1089/dia.2020.0619. file:///C:/Users/ask2k/Downloads/dia.2020.0619%20(3).pdf
- Nevo-Shenker M, Phillip M, Nimri R, Shalitin S. Type 1 diabetes mellitus management in young children: implementation of current technologies. Pediatr Res. 2020;87(4):624-629.
- Buckingham BA, Cameron F, Calhoun P, et al. Outpatient safety assessment of an in-home predictive low-glucose suspend system with type 1 diabetes subjects at elevated risk of nocturnal hypoglycemia. Diabetes Technol Ther. 2013;15(8):622-627.
- Buckingham BA, Raghinaru D, Cameron F, et al. Predictive low-glucose insulin suspension reduces duration of nocturnal hypoglycemia in children without increasing ketosis. Diabetes Care. 2015;38(7):1197-1204.
- Maahs DM, Calhoun P, Buckingham BA, et al. A randomized trial of a home system to reduce nocturnal hypoglycemia in type 1 diabetes. Diabetes Care. 2014;37(7):1885-1891.
- Battelino T, Nimri R, Dovc K, Phillip M, Bratina N. Prevention of hypoglycemia with predictive low glucose insulin suspension in children with type 1 diabetes: A randomized controlled trial. Diabetes Care. 2017;40(6):764-770.
- Zhong A, Choudhary P, McMahon C, et al. Effectiveness of automated insulin management features of the MiniMed ® 640G sensor-augmented insulin pump. Diabetes Technol Ther. 2016;18(10):657-663.
- Hovorka R, Elleri D, Thabit H, et al. Overnight closed-loop insulin delivery in young people with type 1 diabetes: a free-living, randomized clinical trial. Diabetes Care. 2014;37(5):1204-1211.
- Leelarathna L, Dellweg S, Mader JK, et al. Day and night home closed-loop insulin delivery in adults with type 1 diabetes: three-center randomized crossover study. Diabetes Care. 2014;37(7):1931-1937.
- Nimri R, Muller I, Atlas E, et al. MD-Logic overnight control for 6 weeks of home use in patients with type 1 diabetes: randomized crossover trial. Diabetes Care. 2014;37(11):3025-3032.
- Thabit H, Tauschmann M, Allen JM, et al. Home use of an artificial beta cell in type 1 diabetes. N Engl J Med. 2015;373(22):2129-2140.
- Del Favero S, Place J, Kropff J, et al. Multicenter outpatient dinner/overnight reduction of hypoglycemia and increased time of glucose in target with a wearable artificial pancreas using modular model predictive control in adults with type 1 diabetes. Diabetes Obes Metab. 2015;17(5):468-476.
- Saunders A, Messer LH, Forlenza GP. MiniMed 670G hybrid closed loop artificial pancreas system for the treatment of type 1 diabetes mellitus: overview of its safety and efficacy. Expert Rev Med Devices. 2019;16(10):845-853.
- Spaic T, Driscoll M, Raghinaru D, et al. Predictive hyperglycemia and hypoglycemia minimization: In-home evaluation of safety, feasibility, and efficacy in overnight glucose control in type 1 diabetes. Diabetes Care. 2017;40(3):359-366.
- Haidar A, Messier V, Legault L, Ladouceur M, Rabasa-Lhoret R. Outpatient 60-hour day-and-night glucose control with dual-hormone artificial pancreas, single-hormone artificial pancreas, or sensor-augmented pump therapy in adults with type 1 diabetes: An open-label, randomised, crossover, controlled trial. Diabetes Obes Metab. 2017;19(5):713-720.
- Haidar A, Rabasa-Lhoret R, Legault L, et al. Single- and dual-hormone artificial pancreas for overnight glucose control in type 1 diabetes. J Clin Endocrinol Metab. 2016;101(1):214-223.
- Blauw H, Keith-Hynes P, Koops R, DeVries JH. A review of safety and design requirements of the artificial pancreas. Ann Biomed Eng. 2016;44(11):3158-3172.
- El-Khatib FH, Balliro C, Hillard MA, et al. Home use of a bihormonal bionic pancreas versus insulin pump therapy in adults with type 1 diabetes: a multicentre randomised crossover trial. Lancet. 2017;389(10067):369-380.
- Weisman A, Bai JW, Cardinez M, Kramer CK, Perkins BA. Effect of artificial pancreas systems on glycaemic control in patients with type 1 diabetes: a systematic review and meta-analysis of outpatient randomised controlled trials. Lancet Diabetes Endocrinol. 2017;5(7):501-512.
- Bally L, Thabit H, Kojzar H, et al. Day-and-night glycaemic control with closed-loop insulin delivery versus conventional insulin pump therapy in free-living adults with well controlled type 1 diabetes: an open-label, randomised, crossover study. Lancet Diabetes Endocrinol. 2017;5(4):261-270.
- Taleb N, Coriati A, Khazzaka C, Bayonne J, Messier V, Rabasa-Lhoret R. Stability of commercially available glucagon formulation for dual-hormone artificial pancreas clinical use. Diabetes Technol Ther. 2017;19(10):589-594.
- Brown SA, Beck RW, Raghinaru D, et al. Glycemic outcomes of use of CLC Versus PLGS in type 1 diabetes: A randomized controlled trial. Diabetes Care. 2020;43(8):1822-1828.
- Brown SA, Kovatchev BP, Raghinaru D, et al. Six-month randomized, multicenter trial of closed-loop control in type 1 diabetes. N Engl J Med. 2019;381(18):1707-1717.