Peer Reviewed
At any of the over 26,000 restaurants that populate the city of New York, I have to ask the same questions: “Does this have dairy in it? What about gluten?” For my older brother, the list of questions grows to include beans, artificial sweeteners, and all manners of cruciferous vegetables. After being plagued by chronic abdominal distress for much of our early childhood, our diagnosis of irritable bowel syndrome (IBS) was not surprising. Yet our understanding of IBS as a “brain-gut” disorder, or that depression and anxiety may be tied to it, eluded us.
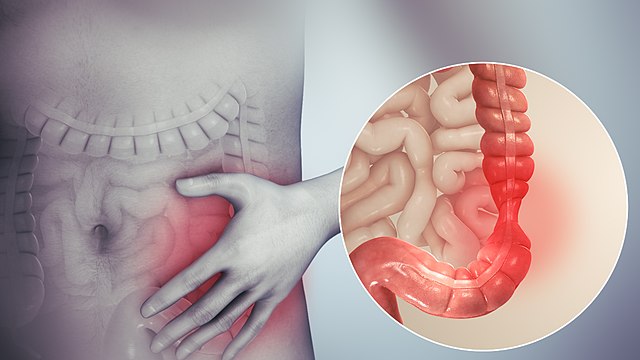
IBS affects anywhere from 7% to 16% of people in the US, costing Americans upwards of $1 billion every year in direct healthcare costs.1 IBS is widely known as a functional bowel disorder characterized by abdominal pain, bloating, distention, and bowel habit abnormalities.2 Diagnosis by the Rome IV criteria requires recurrent abdominal pain at least 1 day per week for 3 months, associated with at least 2 of the following: pain related to defecation, pain associated with a change in frequency of stool, or pain associated with a change in form of stool. The Rome IV criteria further divide IBS into 3 subtypes according to the predominant bowel habit abnormality: IBS with predominant constipation, IBS with predominant diarrhea, and IBS with mixed bowel habits.3 The diagnosis of IBS is made by a careful history as patients report pain, irregular bowel habits, and either symptoms of chronic constipation, unpredictable patterns of diarrhea, or a mix of both. Rectal examination, ultrasonography, and/or the Bristol Stool Form Scale4 often lead to a diagnosis without the need for extensive laboratory testing.1,5
For many patients and practitioners, diagnostic focus on abdominal symptoms, abdominal physical exam findings, and laboratory testing seem to solidify IBS as a purely gastrointestinal syndrome. However, it is now evident that irritable bowel syndrome is not simply a functional gastrointestinal disorder but instead a complex interaction between the microbiota, immune system, and autonomous nervous system. The core signaling pathway between the gut microbiota and the autonomous nervous system is called the gut-brain axis (GBA).6 This GBA encompasses the neuroendocrine and neuroimmune systems, the sympathetic and parasympathetic arms of the autonomic nervous system, the enteric nervous system, and the intestinal microbiota. This interconnection is bidirectional, with efferent fibers influencing motor, sensory, and secretory functions of the gastrointestinal tract and afferent fibers influencing brain function.7
Most patients with IBS have instability of their intestinal microbiota as well as reduced microbiota diversity.8 In addition, the enteric immune system of patients with IBS is disrupted. Low-grade inflammation predominates all forms of IBS with an increase in mast cells, eosinophils, and intraepithelial lymphocytes that lead to visceral hypersensitivity, epithelial and neuromuscular dysfunction, and altered peristalsis.9 Furthermore, since the autonomic nervous system communicates with the intestinal tract and intestinal microbiota via enteric, spinal, and basal pathways, stress plays a large role in the release of stress-related hormones (epinephrine, norepinephrine, and corticotropin-releasing factor)10 that interfere with the functioning of the intestinal tract in patients with IBS.6 The influence of stress on intestinal function suggests that anxiety and depression may themselves lead to IBS in a top-down fashion (brain to gut).
These pathophysiological changes are now being connected to the physiological comorbidities associated with IBS in a bottom-up fashion (gut to brain). Microbiota transplantation from IBS patients with anxiety into mice triggered increased intestinal transit, loss of barrier function, immune activation, and anxiety-like behaviors. Bacterial metabolic pathways have been shown to affect neurotransmitter systems as well as human metabolic and epigenetic effects that impact social cognition, reward, and emotion processing.11 Understanding these mechanisms may shed light on the increased prevalence of comorbid depression and anxiety found in patients with IBS. Patients with IBS of all subtypes were found to have significantly higher anxiety and depression levels compared with control groups, making depression and anxiety key comorbid conditions to look for in patients with IBS.12
A complete understanding of IBS as not only a functional gastrointestinal disorder, but a complex disorder of the brain-gut axis and its interacting domains of microbiota, immune system, and autonomous nervous system are key to improving treatment and identifying comorbid depression and anxiety. Future research will likely shed light on treatments focused on this gut-brain axis that will treat not only the gastrointestinal components of the disorder, but the psychological comorbidities as well.
Quinn Silverglate is a 2nd year medical student at NYU Grossman School of Medicine
Peer reviewed by Michael Tanner, MD, associate editor, Clinical Correlations
Image courtesy of Wikimedia Commons, source: http://www.scientificanimations.com/
References
- Casen C, Vebø H, Sekelja M, et al. Deviations in human gut microbiota: a novel diagnostic test for determining dysbiosis in patients with IBS or IBD. Aliment Pharmacol Ther. 2015;42(1):71-83. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5029765/
- Ford AC, Lacy BE, Talley NJ. Irritable bowel syndrome. N Engl J Med. 2017;376(26):2566-2578. doi:10.1056/NEJMra1607547
- Rome IV Criteria. Rome Foundation website. Published October 19, 2020. Accessed September 2, 2021. https://theromefoundation.org/rome-iv/rome-iv-criteria/
- Lewis SJ, Heaton KW. Stool form scale as a useful guide to intestinal transit time. Scand J Gastroenterol. 1997;32(9):920-924. doi:10.3109/00365529709011203
- Fond G, Loundou A, Hamdani N, et al. Anxiety and depression comorbidities in irritable bowel syndrome (IBS): a systematic review and meta-analysis. Eur Arch Psychiatry Clin Neurosci. 2014;264(8):651-660.
- Grenham S, Clarke G, Cryan JF, Dinan TG. Brain-gut-microbe communication in health and disease. Front Physiol. 2011;2:94. doi:10.3389/fphys.2011.00094 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3232439/
- Holtmann GJ, Ford AC, Talley NJ. Pathophysiology of irritable bowel syndrome. Lancet Gastroent Hepatol. 2016;1(2):133-146.
- Lacy BE, Mearin F, Chang L, et al. Bowel disorders. Gastroenterology. 2016;150(6):1393-1407. e5.
- Peter J, Fournier C, Durdevic M, et al. A microbial signature of psychological distress in irritable bowel syndrome. Psychosom Med. 2018;80(8):698-709. https://pubmed.ncbi.nlm.nih.gov/30095672/
- Bhatia V, Tandon RK. Stress and the gastrointestinal tract. J Gastroenterol Hepatol. 2005;20(3):332-339. doi:10.1111/j.1440-1746.2004.03508.x
- Raskov H, Burcharth J, Pommergaard H-C, Rosenberg J. Irritable bowel syndrome, the microbiota and the gut-brain axis. Gut Microbes. 2016;7(5):365-383. doi:10.1080/19490976.2016.1218585 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5046167/
- Wouters MM, Vicario M, Santos J. The role of mast cells in functional GI disorders. Gut. 2016;65(1):155-168.