Peer Reviewed
The default mode of medical practice is curative: pursuit of the complete eradication of the malady at hand, leading to symptomatic relief and prolongation of life. In actuality, this frame is more aspirational than reality-based. Physicians quickly learn to confront difficult-to-treat diseases with realistic expectations. This principle of tempered expectations extends to patients as well, who frequently may not live the healthy lifestyles medical textbooks dictate. Patients have complex motivations for their health behaviors, rooted in deep-seated socialization that can sometimes be impossible to upend. As the tendency to meet patients where they are, rather than where physicians believe they should be, becomes more widespread, so too does the “harm reduction” approach to health interventions.
What precisely do practitioners mean when they discuss harm reduction? Harm Reduction International defines it as “policies, programs, and practices that aim to minimize negative health, social and legal impacts associated with drug use, drug policies and drug laws.”1 However, the National Harm Reduction Coalition cautions that “there is no universal definition of or formula for implementing harm reduction.”2
Approaching harm reduction through the lens of drug use makes intuitive sense. The harm reduction approach to addiction takes a reality-based approach, accepting that some patients may never fully abstain from drug use, and working instead to mitigate the associated harms. This stands in stark contrast to a model of addiction that suggests that drug use is somehow “wrong” and must be entirely stamped out. However, this limits the frame of harm reduction to practices surrounding drug use alone, a critical but narrow slice of this far-reaching approach.
Harm reduction, then, can be approached as a set of principles that guide the development of specific policies rather than a concrete set of actionable practices. Hawk and colleagues conducted systematic interviews with the staff and patients of an HIV clinic that implemented harm reduction protocols.3 Many of the clinic’s patients came from populations where outcomes are often poorer (the housing unstable, psychiatrically ill, etc.), but the clinic had particularly high success rates, with 95% of patients being prescribed anti-retroviral therapy and 87% reaching undetectable viral loads. The researchers sought an explanation for these successes and distilled their findings into broad principles for harm reduction.
At baseline, they note, providers must “value, care for, respect, and dignify patients as individuals,” while accepting that “patients have reasons for engaging in harmful behaviors.” This practice of humanism (Principle #1), where moral judgements do not affect health outcomes, is critical to implementing health justice. Pragmatism, the notion that “no one will ever engage in perfect health behaviors” and that “health behaviors are influenced by community norms” plays a similar role in the harm reduction frame (Principle #2). In this clinic’s experience, pragmatic providers did not presume that abstinence from poor health behaviors was the goal of treatment, and honed care messages to describe actual harms, rather than social norms. Patients must also be approached with individualism in mind, the notion that a given patient requires a “spectrum of treatment options tailored to their unique characteristics” (Principle #3). In practice, providers can assess each patient’s strengths in an effort to avoid universal messaging tactics that too frequently fall on deaf ears.
Interviewees also described how preserving patient autonomy–educating and advising patients on best tactics, while allowing patients to “make ultimate choices according to their own priorities”–led to the development of rich provider-patient relationships that could be leveraged to promote healthy decision-making (Principle #4). However, progress in reducing harms cannot be expected to occur overnight. With an incremental approach, providers appreciate that “any positive change,” no matter how seemingly insignificant, is a “step toward improvement,” but “backsliding” must be anticipated and planned for (Principle #5). In this light, patients must come to expect “accountability without termination,” that is, “patients are [held] responsible for their choices, but are not cut off from care when they fail” (Principle #6). It is the provider’s role to educate around failures, providing meaningful reinforcement and actionable next steps, instead of resorting to “punishment” in these circumstances.
How can we implement these six principles of harm reduction–humanism, pragmatism, individualism, autonomy, incrementalism, and accountability without termination–into both clinical practice and broader social policy? Guided by this frame, advocates for the harm reduction approach to opioid use disorder have already made significant headway in popularizing lifesaving interventions such as opioid replacement therapy, safe injection sites, and needle exchange programs. Encouragingly, researchers, clinicians, and activists have begun to take the first steps into expanding this approach into other domains.
Harm reduction principles certainly have a place in social policy. Beginning in the 1980s, governments around the world implemented HIV-control programs centered on commercial sex. Rather than initiating a quixotic campaign to eliminate sex work, the government of Thailand pragmatically sought to reduce the associated harms. Sanctions were brought against establishments where condoms were not used consistently, and a media campaign advised men to use condoms with sex workers. This approach was highly effective: condom use skyrocketed, from 14% to 93% in the period from 1989 to 1993.4 By 2002, Thailand had avoided an estimated 5.7 million HIV infections.
In a 1998 study, one Thai group sought to evaluate whether harm reduction interventions that empower sex workers, protect their autonomy, and provide an individualized slate of options have higher rates of uptake.5 249 women in 34 sex establishments were provided with male and female condoms, while 255 women in 37 sex establishments were provided with male condoms alone. The researchers hypothesized that access to the female condom would allow these women a greater deal of control over decisions surrounding barrier use, which had previously been dominated by men. Accordingly, there was a 17% reduction in the reported number of unprotected sex acts in the group with access to the female condom and a 24% reduction in the mean incidence rate of STIs when compared to the male-condom-only group.
The frontiers of the harm reduction approach extend beyond social policy. Some experts have hypothesized a codified harm reduction framework for engagement with patients with severe and enduring eating disorders.6 These patients are frequently subjected to an extensive course of treatment that involves frequent hospital stays, inpatient rehabilitation, and close outpatient follow-up. Owing to the precarious nature and high acuity of this condition, these interventions often aim toward the restoration of ideal body weight. However, some patients repeatedly relapse, despite extensive first-line interventions. These patients in particular may benefit from a harm reduction approach.
Perhaps, some have suggested, clinicians should approach these cases pragmatically, accepting that maintenance of ideal body weight is an unattainable goal.7 Instead, perhaps an individualized weight range can be determined wherein a patient can medically stabilize and have a moderate quality of life, even if they cannot work or be fully independent. Frequent outpatient follow-up and monitoring of basic metabolic parameters can trigger hospital admission in the event of deviation from an agreed-upon range. Such deviations would result in accountability during the hospitalization process, but without “punishment” or termination of care.
The harm reduction frame is an appropriate approach for an imperfect world. Clinicians must recognize that mitigation of further damage is every bit as central to their role as full-blown cure. With the above principles in mind, providers and policymakers alike can make informed decisions that are grounded in the realities patients experience, instead of centering on unattainable aspirations.
Matthew Haller is a 2nd year medical student at NYU Grossman School of Medicine
Reviewed by Michael Tanner, MD, associate editor, Clinical Correlation
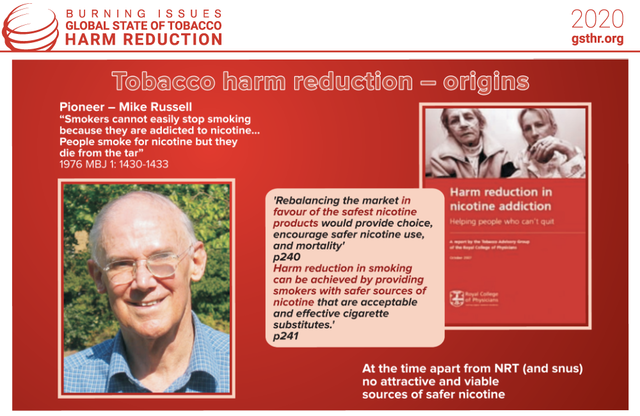
Image courtesy of Wikimedia Commons, source: Tobacco Harm Reduction – Origins.png
File:Tobacco Harm Reduction – Origins.png|Tobacco_Harm_Reduction_-_Origins
References
- Harm Reduction Coalition. Principles of harm reduction. https://harmreduction.org/about-us/principles-of-harm-reduction Accessed May 28, 2021.
- International Harm Reduction Association. What is harm reduction? https://www.hri.global/what-is-harm-reduction Published 2021. Accessed May 28, 2021.
- Hawk M, Coulter RWS, Egan JE, et al. Harm reduction principles for healthcare settings. Harm Reduct J. 2017;14(1):70.
- Hanenberg RS, Rojanapithayakorn W, Kunasol P, Sokal DC. Impact of Thailand’s HIV-control programme as indicated by the decline of sexually transmitted diseases. Lancet. 1994;344(8917):243-245. https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(94)93004-X/fulltext
- Fontanet AL, Saba J, Chandelying V, et al. Protection against sexually transmitted diseases by granting sex workers in Thailand the choice of using the male or female condom: results from a randomized controlled trial. AIDS. 1998;12(14):1851-1859.
- Westmoreland P, Mehler P. Caring for patients with severe and enduring eating disorders (SEED): Certification, harm reduction, palliative care, and the question of futility. J Psychiatr Pract. 2016;22(4):313-320. https://pubmed.ncbi.nlm.nih.gov/27427843/
- Robinson P. Severe and enduring eating disorders: recognition and management. Adv Psychiatric Treatment. 2014;20:392-401. https://www.cambridge.org/core/journals/advances-in-psychiatric-treatment/article/severe-and-enduring-eating-disorders-recognition-and-management/8A318F286A6F12888B3FD3AB8FCD6846