Peer Reviewed
I caught up with a friend who works in environmental, social, and corporate governance investing during a lull in the COVID-19 pandemic. Seconds into the conversation, he asked, “I hear the future is precision medicine, that they will just take a blood sample and tell you everything you need to do for your health. What do you think? Is it feasible?” The question brought to mind Theranos’s failed lab-on-a-chip, yet aspects of personalized medicine are being incorporated more and more into medical practice, from the Deterioration Index implemented in the electronic health record (EHR) at NYU in the midst of the pandemic to increasingly advanced profiling of cancer genetics, epigenetics, and histopathology.1-3 Such innovations raise the question of where precision medicine intersects with everyday practice.
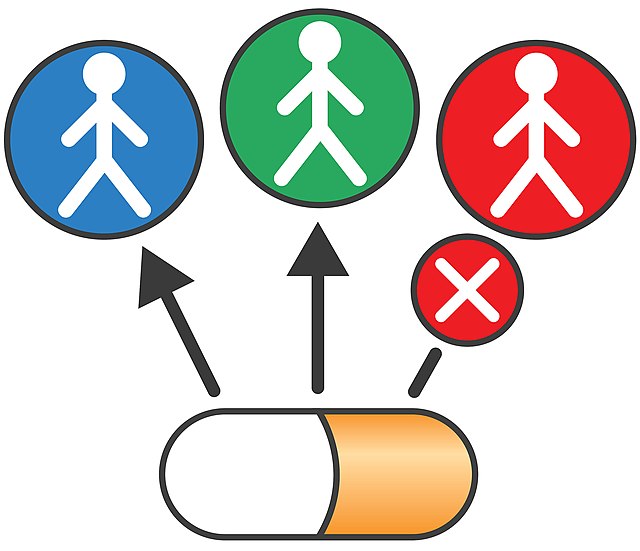
The idea of precision medicine, defined by the NIH as “an approach for disease prevention and treatment that takes into account individual variations in genes, environment, and lifestyle,” is not new.4 For example, after the discovery of the amino acid sequence of insulin in 1951, recombinant human insulin was produced nearly three decades later and is integral to the management of diabetes.5,6 Moreover, the latter half of the 20th century following the discovery of DNA brought a revolution in molecular biology. With the success of imatinib (Gleevec) in directly targeting the oncogene BCR-ABL in chronic myeloid leukemia, and the completed sequencing of the human genome, the turn of the 21st century brought the promise of therapeutic efforts targeted to individual genomes that would “boost effectiveness while drastically reducing side effects.”7-10 While mapping the human genome did support the development of novel therapies, such as the recently FDA-approved gene therapy for Duchenne muscular dystrophy, precision medicine remains laborious, time-intensive, and expensive. The median cost of bringing a new therapeutic agent to market continues to soar, estimated around 1 billion US dollars in 2020.11,12
Paralleling the major discoveries in molecular biology, another revolution was brewing in the late 20th and early 21st centuries. Machine learning, defined as the automation of building an algorithm, was first developed in the 1960s, and by the 1980s the foundations of today’s neural networks were developed.13 A neural network is a set of interconnected processors, or “neurons,” each activated at different stages of the computation to provide inputs towards the final “learning.”14 Deep learning consists of providing the computer with raw data (often with labels, ie, supervision) to learn an algorithm that predicts the labels of the data through a neural network, where “neurons” are organized hierarchically.13,14 In the late 2000s, the foundations of what would become the deep learning methods underlying modern image (eg, face recognition), language (eg, Google translate) and speech recognition (eg, Siri) were developed.13 With technological advances enabling higher storage and RAM capacity meeting advances in the architecture and methods of training neural networks, deep learning is increasingly applied to solve problems of classification in medicine.
Deep learning has been leveraged in numerous clinical applications, for example, predicting response to immunotherapy in melanoma, lung cancer mutations from histopathology slides, and lung cancer from low-dose chest computed tomography images.15-17 Nearly 200 artificial intelligence (AI) algorithms related to radiology and imaging have been approved by the FDA.18 Indeed, deep learning is poised to address some of the barriers to precision medicine, including analyzing the wealth of data available and identifying relationships between human health and the contents of the EHR.13,19 However, such studies require large sets of data on which to train and extensive effort from computational biologists, pathologists, etc.13,14 An additional challenge for machine learning algorithms is improving transferability to different scenarios, which limits the broad applicability of these studies.20 Thus, further development of both available data and neural networks is needed to augment transferability and interpretability of deep learning applications in the clinical setting.20 With recent advances in the quality and cost of data acquisition, expanding numbers of high-quality large datasets are being developed, some of which are publicly available. In addition, an increasing abundance of peer-reviewed supervised and unsupervised machine learning algorithms are being applied to diverse clinical scenarios involving diagnosis, therapy, and health maintenance.21 Thus, given the convergence of the availability of high-quality datasets and the enhanced performance and applicability of neural networks, deep learning is poised to potentially address diverse clinical problems in precision medicine.
Where does precision medicine deep learning fit within primary care? The primary care physician already leverages precision medicine when treating distinct patients with varying numbers and doses of medications to achieve goal blood pressure, hemoglobin A1c, low-density lipoprotein cholesterol, etc. They engage the patient as an individual and build a longitudinal relationship to optimize the patient’s medical care. With regard to deep learning, the primary care physician uses some algorithms and applications to enhance their practice. The EHR includes recommendations for US Preventive Services Task Force guidelines and notifies the care provider of overdue immunizations or screenings. In addition, a physician can use a smart phrase to calculate the 10-year atherosclerotic cardiovascular disease risk within the chart. Moreover, the auto-population of immunization information into the EHR after a vaccine card has been scanned relies on image and language recognition through deep learning.13
As the EHR is more widely adopted and utilized, standardization of interpretation of the EHR and integration with available genomic, proteomic, and/or metabolomic analysis is critical.19 The EHR impedes analysis in that it was designed for billing rather than documenting medical and biological features of the patient.19 Often, terminology between physicians varies and the EHR can have varying degrees of complete information.19 Deep learning harbors the potential not only to parse the information derived from the EHR but also to leverage language, image, and speech recognition to maintain humanistic patient interviews while achieving completeness in documentation.13,19 As diagnostic tests become increasingly advanced, deep learning could also help identify disease ontology relationships to enhance diagnosis.22
Important considerations to the ethics and applicability of deep learning must be made as the revolutions of precision medicine and computational power intersect. First, deep learning relies on natural signals within complex hierarchies and thus it has the potential to amplify pre-existing healthcare disparities.13,20 This raises critical questions of how to balance supervision in the learning process with computational feasibility and power to prevent propagation of inequality in medicine. In addition, what level of informed consent is needed for patients to agree to use of their EHR in the future for deep learning? New legislation is likely needed to ensure patient privacy and protection in the era of omics data and the EHR. In addition, how deep learning can effectively benefit the humanism of the physician-patient relationship is critical. Imagine during the patient interview the chief complaint, history of present illness, family history, etc. auto-populated in the EHR through language recognition. Would this help or harm the relationship? What about the patient? Randomized trials are needed to make deep learning in healthcare more broadly applicable.20,22 At this time, few prospective studies or randomized trials exist in deep learning, and most studies are at risk of bias and do not make data and code readily available.22 For these reasons, human oversight will be integral to bringing AI algorithms into more mainstream use.
To return to the question at hand: are pan-diagnostic blood tests in our near future? For the time being, the answer is no. However, the NIH Precision Medicine Initiative together with advancements in diagnostic and computational technology are charging ahead towards changing the practice of medicine. Accumulating studies demonstrate progress towards the incorporation of supervised and unsupervised machine learning into diagnosis and treatment. Important questions must be raised regarding the ethics, the reproducibility, the allocation of resources, the promotion of diversity… However, the history of medicine is replete with unexpected discoveries and detours, so this level of precision medicine is likely to come to fruition.
The future is too interesting and dangerous to be entrusted to any predictable, reliable agency. We need all the fallibility we can get. Most of all, we need to preserve the absolute unpredictability and total improbability of our connected minds.
–Lewis Thomas, The Lives of a Cell
Kathryn Hockemeyer is a 4th year medical student at NYU Grossman School of Medicine
Reviewed by Marc Triola, MD, Department of Medicine, NYU Langone Health
Image courtesy of Wikimedia Commons, source: File:Personalized Medicine and Companion Diagnostics Go Hand-in-Hand.jpg
References
- Shamout FE, Shen Y, Wu N, et al. An artificial intelligence system for predicting the deterioration of COVID-19 patients in the emergency department. NPJ Digit Med. 2021;4(1):80. doi:10.1038/s41746-021-00453-0 https://www.nature.com/articles/s41746-021-00453-0
- Prasad V, Fojo T, Brada M. Precision oncology: origins, optimism, and potential. Lancet Oncol. 2016;17(2):e81-e86. doi:10.1016/S1470-2045(15)00620-8
- Boehm KM, Khosravi P, Vanguri R, Gao J, Shah SP. Harnessing multimodal data integration to advance precision oncology. Nat Rev Cancer. 2022;22(2):114-126. doi:10.1038/s41568-021-00408-3
- Collins FS, Varmus H. A new initiative on precision medicine. N Engl J Med. 2015;372(9):793-795. doi:10.1056/NEJMp1500523 https://www.nejm.org/doi/full/10.1056/nejmp1500523
- Sanger F, Tuppy H. The amino-acid sequence in the phenylalanyl chain of insulin. 2. The investigation of peptides from enzymic hydrolysates. Biochem J. 1951;49(4):481-490. doi:10.1042/bj0490481
- Goeddel DV, Kleid DG, Bolivar F, et al. Expression in Escherichia coli of chemically synthesized genes for human insulin. Proc Natl Acad Sci U S A. 1979;76(1):106-110. doi:10.1073/pnas.76.1.106
- Druker BJ, Talpaz M, Resta DJ, et al. Efficacy and safety of a specific inhibitor of the BCR-ABL tyrosine kinase in chronic myeloid leukemia. N Engl J Med. 2001;344(14):1031-1037. doi:10.1056/NEJM200104053441401 https://pubmed.ncbi.nlm.nih.gov/11287972/
- Lander ES, Linton LM, Birren B, et al. Initial sequencing and analysis of the human genome. Nature. 2001;409(6822):860-921. doi:10.1038/35057062
- Venter JC, Adams MD, Myers EW, et al. The sequence of the human genome. Science. 2001;291(5507):1304-1351. doi:10.1126/science.1058040
- Lemonick MD. The genome is mapped. Now what? It will be decades before scientists identify and understand all of our genes. But that hasn’t stopped them from making dramatic discoveries. Time. 2000;156(1):24-29.
- Clemens PR, Rao VK, Connolly AM, et al. Safety, tolerability, and efficacy of viltolarsen in boys with duchenne muscular dystrophy amenable to exon 53 skipping: a phase 2 randomized clinical trial. JAMA Neurol. 2020;77(8):982-991. doi:10.1001/jamaneurol.2020.1264 https://pubmed.ncbi.nlm.nih.gov/32453377/
- Wouters OJ, McKee M, Luyten J. Estimated research and development investment needed to bring a new medicine to market, 2009-2018. JAMA. 2020;323(9):844-853. doi:10.1001/jama.2020.1166
- LeCun Y, Bengio Y, Hinton G. Deep learning. Nature. 2015;521(7553):436-444. doi:10.1038/nature14539
- Schmidhuber J. Deep learning in neural networks: an overview. Neural Netw. 2015;61:85-117. doi:10.1016/j.neunet.2014.09.003
- Johannet P, Coudray N, Donnelly DM, et al. Using machine learning algorithms to predict immunotherapy response in patients with advanced melanoma. Clin Cancer Res. 2021;27(1):131-140. doi:10.1158/1078-0432.CCR-20-2415
- Coudray N, Ocampo PS, Sakellaropoulos T, et al. Classification and mutation prediction from non-small cell lung cancer histopathology images using deep learning. Nat Med. 2018;24(10):1559-1567. doi:10.1038/s41591-018-0177-5
- Ardila D, Kiraly AP, Bharadwaj S, et al. End-to-end lung cancer screening with three-dimensional deep learning on low-dose chest computed tomography. Nat Med. 2019;25(6):954-961. doi:10.1038/s41591-019-0447-x
- Wald C, Allen B, Agarwal S, Bizzo BC, Gichoya JW, Patti J. American College of Radiology Data Science Institute AI Central website. https://aicentral.acrdsi.org Accessed 20 Aug 2022.
- Haendel MA, Chute CG, Robinson PN. Classification, ontology, and precision medicine. N Engl J Med. 2018;379(15):1452-1462. doi:10.1056/NEJMra1615014
- Topol EJ. High-performance medicine: the convergence of human and artificial intelligence. Nat Med. 2019;25(1):44-56. doi:10.1038/s41591-018-0300-7
- Goecks J, Jalili V, Heiser LM, Gray JW. How machine learning will transform biomedicine. Cell. 2020;181(1):92-101. doi:10.1016/j.cell.2020.03.022
- Nagendran M, Chen Y, Lovejoy CA, et al. Artificial intelligence versus clinicians: systematic review of design, reporting standards, and claims of deep learning studies. BMJ. 2020;368:m689. doi:10.1136/bmj.m689