Peer Reviewed
“Too many complex back surgeries are being performed and patients are suffering as a result” wrote National Public Radio health science journalist Joanne Silberner in her 2010 article “Surgery May Not Be The Answer To An Aching Back”.1 This quote was in response to a manuscript by Deyo and colleagues in JAMA that found that lumbar fusion, one of the most commonly performed spine surgeries for low back pain, provided little benefit to patients and was in fact associated with high rates of major complications including infections, pulmonary embolism, and even mortality.2,3 So what is the role of spine surgery in low back pain?
Low back pain is the leading cause of limited physical activity and absence from work in much of the world.4,5 It is estimated that 30% of the US population will experience disabling low back pain in any given year and 65-80% will experience it in their lifetimes.6 The factors that lead to its development remain incompletely understood.7 Potential causes of low back pain range from degenerative disk disease to trauma and psychological factors such as stress.8 A common treatment for patients with chronic low back pain who fail conservative therapy is spine surgery, most commonly a procedure called a spinal fusion.9
Spinal fusion consists of placing bone or bone-like material between two or more vertebrae that eventually grows over time to “fuse” the vertebrae together. The rationale behind spinal fusion is that unstable spinal motion may be at the root of the patient’s pain and thus fused vertebrae that cannot move should not generate back pain. This surgery was initially used for the treatment of severe scoliosis, spinal tuberculosis, and fractures. Now, however, approximately 75% of spinal fusions are performed for degenerative changes of the spine and spinal stenosis.3 Due to advances in surgical implant design, fusions began being routinely used to treat degenerative disk disease of the spine in the 1990s, leading to a 220% increase in the number of fusions performed from 1990 to 2001.10,11 Since the early 2000s, the number of fusion surgeries has continued to increase, but at a slower rate.12,13
The use of spinal fusion surgery to treat low back pain has been controversial.14 Despite the increase in the number of spinal fusions over the last three decades, the efficacy of fusion in the treatment of chronic low back pain has been inconclusive. In a systematic review of four randomized controlled trials that compared the outcomes of low back pain patients who had fusion surgery versus those who had nonoperative care, only one of the trials showed improvement in the operative group, while the other three showed no difference.15 Another cause for concern with spinal fusion is the relatively high rate of reoperation associated with the procedure, which has been reported to be as high as 14%.16 One of the most dreaded consequences of this continued reoperation is “failed back syndrome,” a term that refers to low back pain that persists or increases following multiple spine surgeries. Patients with failed back syndrome are often consigned to a life of long-term narcotic treatment with little chance of recovery.17
Although the benefit of spine surgery in chronic nonspecific low back pain is unclear, there are several conditions for which spine surgery demonstrates a clear advantage over conservative therapy. The Spine Patient Outcomes Research Trial (SPORT) was a randomized-plus-observational cohort trial of 2500 patients that compared outcomes of spine surgery versus non-operative care in patients with three of the most common pathological spine diagnoses: spinal stenosis, degenerative spondylolisthesis, and intervertebral disk herniation.18-20 One of the outcomes reported in this trial comparing surgical treatment and nonoperative care was quality adjusted life years (QALYs), a metric that accounts for changes in both length and quality of life for a given medical intervention.
The 6/20/20 issue of Spine reported back-to-back-to-back analyses of the three major SPORT trial operations at the 10-year follow-up mark. Patients who underwent surgery had persistent improvement in QALYs over non-operatively treated patients, as follows: spinal stenosis QALY gain 0.22, 95% CI 0.15-0.34; degenerative spondylolisthesis QALY gain 0.34, 95% CI: 0.30-0.47; herniated disk QALY gain 0.34, 95% CI 0.31-0.38). Other outcomes measured in this study included recovery time, physical functioning, pain, and satisfaction. Patients with intervertebral disk herniation who underwent surgery had more rapid recovery, better results in physical functioning, and improved satisfaction at one and two years follow-up when compared to the nonoperative group.21 Patients with spinal stenosis who were treated surgically showed significantly greater improvement in pain and physical functioning through 2 years follow-up compared to patients treated nonsurgically.22 The results for the degenerative spondylolisthesis group showed substantial pain relief and improvement in physical function at four years follow-up. 23
Additionally, a systematic review conducted by Teles and colleagues of operative versus nonoperative care in patients with adult spinal deformity and low back pain showed the superiority of surgery over conservative management.24 Patients with adult spinal deformity who underwent surgery had a substantial improvement in back pain, level of disability, and quality of life, while nonoperative care did not demonstrate any significant changes in quality of life at 2 years follow-up. However, the study did find the average revision rate for the adult spinal deformity surgery was relatively high at 15.2%.
Finally, there are several acute and more serious types of low back pain for which spine surgery has been widely accepted as a necessity, including tumors compressing the spinal cord and nerve roots, trauma causing instability of the spine, and infection of the spine.25-27 These indications for spine surgery are regarded as uncontroversial, as not intervening surgically could lead to permanent neurological deficit or death.28-30
While spinal fusion surgery for chronic nonspecific low back pain has provided inconclusive outcomes and may be of limited benefit for most patients, there are many diagnosable spinal pathologies for which surgery has been shown to be advantageous over nonoperative treatment. Patients who have severe and symptomatic intervertebral disk herniations, spinal stenosis, degenerative spondylolisthesis and adult spinal deformity refractory to conservative therapy should be considered candidates for spine surgery. Additionally, patients with acute and life-threatening spine pathologies including spine tumors, trauma and infection should always be considered for surgery.
Michael Moore is a Class of 2024 medical student at NYU Grossman School of Medicine
Peer reviewed by Michael Tanner, MD, Associate Editor, Clinical Correlations
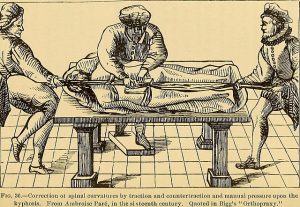
Image courtesy of Wikimedia Commons from Book: Lectures on Orthopedic Surgery Authors Ridlon John, Thomas Hugh Owen, Jones, Robert 1899
References
- Silberner J. Surgery may not be the answer to an aching back. National Public Radio. April 6, 2010. https://www.npr.org/templates/story/story.php?storyId=125627307.) Accessed January 27, 2022.
- Daniell JR, Osti OL. Failed back surgery syndrome: A review article. Asian Spine J 2018;12(2):372-379.
- Deyo RA, Nachemson A, Mirza SK. Spinal-fusion surgery–the case for restraint. N Engl J Med. 2004;350(7):722-726.
- Minghelli B. Musculoskeletal spine pain in adolescents: Epidemiology of non-specific neck and low back pain and risk factors. J Orthop Sci. 2020;25(5):776-780.
- Fatoye F, Gebrye T, Odeyemi I. Real-world incidence and prevalence of low back pain using routinely collected data. Rheumatol Int. 2019;39(4):619-626.
- Urits I, Burshtein A, Sharma M, et al. Low back pain, a comprehensive review: pathophysiology, diagnosis, and treatment. Curr Pain Headache Rep. 2019;23(3):23.
- Popescu A, Lee H. Neck pain and lower back pain. Med Clin North Am. 2020;104(2):279-292.
- DePalma MG. Red flags of low back pain. JAAPA. 2020;33(8):8-11.
- Eichler J, Lenz H. Comparison of different coefficients and units in rhinomanometry. Rhinology. 1985;23(2):149-157.
- Deyo RA, Mirza SK, Turner JA, Martin BI. Overtreating chronic back pain: time to back off? J Am Board Fam Med. 2009;22(1):62-68.
- Martin BI, Mirza SK, Spina N, Spiker WR, Lawrence B, Brodke DS. Trends in lumbar fusion procedure rates and associated hospital costs for degenerative spinal diseases in the United States, 2004 to 2015. Spine (Phila Pa 1976). 2019;44(5):369-376.
- Rajaee SS, Bae HW, Kanim LE, Delamarter RB. Spinal fusion in the United States: analysis of trends from 1998 to 2008. Spine (Phila Pa 1976). 2012;37(1):67-76.
- Reisener MJ, Pumberger M, Shue J, Girardi FP, Hughes AP. Trends in lumbar spinal fusion–a literature review. J Spine Surg. 2020;6(4):752-761.
- Dhillon KS. Spinal fusion for chronic low back pain: a ‘magic bullet’ or wishful thinking? Malays Orthop J. 2016;10(1):61-68.
- Mirza SK, Deyo RA. Systematic review of randomized trials comparing lumbar fusion surgery to nonoperative care for treatment of chronic back pain. Spine (Phila Pa 1976). 2007;32(7):816-823.
- Martin BI, Mirza SK, Comstock BA, Gray DT, Kreuter W, Deyo RA. Are lumbar spine reoperation rates falling with greater use of fusion surgery and new surgical technology? Spine (Phila Pa 1976). 2007;32(19):2119-2126.
- Onesti ST. Failed back syndrome. Neurologist. 2004;10(5):259-264.
- Oster BA, Kikanloo SR, Levine NL, Lian J, Cho W. Systematic review of outcomes following 10-year mark of Spine Patient Outcomes Research Trial (SPORT) for degenerative spondylolisthesis. Spine (Phila Pa 1976). 2020;45(12):820-824.
- Oster BA, Kikanloo SR, Levine NL, Lian J, Cho W. Systematic review of outcomes following 10-year mark of Spine Patient Outcomes Research Trial for intervertebral disc herniation. Spine (Phila Pa 1976). 2020;45(12):825-831.
- Oster BA, Kikanloo SR, Levine NL, Lian J, Cho W. Systematic review of outcomes following 10-year mark of Spine Patient Outcomes Research Trial (SPORT) for spinal stenosis. Spine (Phila Pa 1976). 2020;45(12):832-836.
- Lurie JD, Tosteson TD, Tosteson AN, et al. Surgical versus nonoperative treatment for lumbar disc herniation: eight-year results for the Spine Patient Outcomes Research Trial. Spine (Phila Pa 1976). 2014;39:3-16.
- Weinstein JN, Tosteson TD, Lurie JD, et al. Surgical versus nonoperative treatment for lumbar spinal stenosis four-year results of the Spine Patient Outcomes Research Trial. Spine (Phila Pa 1976). 2010;35(14):1329-1338.
- Weinstein JN, Lurie JD, Tosteson TD, et al. Surgical compared with nonoperative treatment for lumbar degenerative spondylolisthesis. four-year results in the Spine Patient Outcomes Research Trial (SPORT) randomized and observational cohorts. J Bone Joint Surg Am. 2009;91(6):1295-1304.
- Teles AR, Mattei TA, Righesso O, Falavigna A. Effectiveness of operative and nonoperative care for adult spinal deformity: Systematic review of the literature. Global Spine J. 2017;7(2):170-178.
- Babic M, Simpfendorfer CS, Berbari EF. Update on spinal epidural abscess. Curr Opin Infect Dis. 2019;32(3):265-271.
- Joaquim AF, Patel AA, Schroeder GD, Vaccaro AR. A simplified treatment algorithm for treating thoracic and lumbar spine trauma. J Spinal Cord Med. 2019;42(4):416-422.
- Amelot A, Balabaud L, Choi D, et al. Surgery for metastatic spine tumors in the elderly. Advanced age is not a contraindication to surgery! Spine J. 2017;17(6):759-767.
- Mazel C, Balabaud L, Bennis S, Hansen S. Cervical and thoracic spine tumor management: surgical indications, techniques, and outcomes. Orthop Clin North Am. 2009;40(1):75-92, vi-vii.
- Maruo K, Berven SH. Outcome and treatment of postoperative spine surgical site infections: predictors of treatment success and failure. J Orthop Sci. 2014;19(3):398-404.
- Kattail D, Furlan JC, Fehlings MG. Epidemiology and clinical outcomes of acute spine trauma and spinal cord injury: experience from a specialized spine trauma center in Canada in comparison with a large national registry. J Trauma. 2009;67(5):936-943.