Peer Reviewed
You are rounding on your patients, and your team is discussing a 52-year-old man with HIV who came in with shortness of breath and fever and was found to have pneumonia. His roommate, a 67-year-old man whose colorectal cancer is being treated with folinic acid, 5-fluorouracil, and oxaliplatin, presented with diffuse watery diarrhea and is now being treated for Clostridium difficile.
In the next room, you speak with a 66-year-old woman who is preparing to go home after receiving treatment for yet another urinary tract infection, which has become a routine since receiving her living donor kidney transplant two years prior. Despite the repeated infections, the consulted transplant nephrologists are discharging her on the same regimen of prednisone, tacrolimus, and mycophenolate because of their worry about organ rejection.
The team then arrives at the bedside of a 73-year-old woman with type 2 diabetes who developed left ear pain with discharge, mild hearing loss, and headache. Otoscopy revealed granulation tissue in the external auditory canal. A culture of the drainage grew Pseudomonas aeruginosa, confirming the etiology of her malignant otitis externa.
All four patients are immunocompromised and predisposed to infections, but only the first three patients have clear reasons for their immune dysfunction. The man with HIV has a depleted population of CD4+ helper T cells, with impaired cytokine signaling and B cell class switching. The patient with cancer is being treated with chemotherapy, which kills not only his cancer but also his rapidly dividing immune cells. The woman with a kidney transplant is immunosuppressed by the drugs her transplant nephrologists have prescribed.
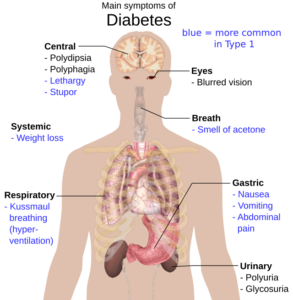
When the attending physician asks why the patient with diabetes is immunocompromised, what is the answer? Diabetes does not interfere with DNA synthesis like 5-fluorouracil or inhibit T cell activation like tacrolimus. Why are common infections such as pneumonia seen more frequently in people with diabetes? Why are diseases like malignant otitis externa or rhino-orbital-cerebral mucormycosis more common in people with diabetes?
Until this century, infection risk in diabetes was exactly like our tour of these patients–anecdotal. A review article published in the New England Journal of Medicine in 1999 began, “Contrary to common belief, the association between diabetes mellitus and increased susceptibility to infection in general is not supported by strong evidence.”1
A study of administrative data in Ontario, Canada changed that.2 The authors compiled all 513,749 people with diabetes as of April Fool’s Day in 1999 who could be matched to other Ontario residents based on age, sex, region, and income. They found a 21% higher risk for infection in people with diabetes.
Another Canadian study matched controls to patients based on age and then adjusted for confounders such as demographics, comorbid conditions, and medications.3 This study reported 21% higher odds of any infection in people with diabetes compared to people without during their study period from 2008-2013.
Meanwhile, a group at St George’s Hospital Medical School in England studied adults aged 40-89 from 2008-2015.4 People with diabetes were matched to people without diabetes based on age, sex, and location and reviewed for whether they had an encounter for an infection in which they were prescribed an antimicrobial. Those with type 1 diabetes had a 66% higher rate of such infections, while those with type 2 diabetes had a 47% higher rate.
These studies answered the question posed in the 1999 review: there is an association between diabetes and susceptibility to infection. They also suggested a new question, which the English study began to investigate: is the association clinically significant?
An early study in the US followed 9208 people aged 30-74 years from 1976 through 1992.5 After adjustments, people with diabetes had a relative risk of death related to infection twice as high as people without diabetes. This increased risk was only seen with people who also had cardiovascular disease at the time of death, as those with diabetes alone had no higher relative risk.
The Emerging Risk Factors Collaboration revisited this question by studying the deaths of 123,205 people among 820,900 participants in 97 prospective studies.6 They found a hazard ratio of 1.67 for a person with diabetes dying from pneumonia. For any other infection, the equivalent number was 2.39. Unlike the first US study, this paper convincingly reported that diabetes is independently associated with death from infection.
How does diabetes mediate this effect? Diabetes is defined by hyperglycemia and its complications, of which microvascular disease is most relevant for infection. People with diabetes often develop vascular insufficiency, which can impair migration and suppress oxygen-dependent immune cell function.7 When systemic antimicrobials are given, they may be less likely to reach the site of infection. People with diabetes are prone to developing sensory peripheral neuropathy, which classically leads to skin ulcers on the feet, sometimes not noticed by the patient until infection occurs.7 Likewise, autonomic neuropathy can predispose to urinary stasis, which leads to urinary tract infections. This may explain why the second Canadian study found that diabetes was most associated with skin, soft tissue, and genitourinary infections.3
Diabetes is also an inflammatory condition. Type 1 diabetes is an autoimmune disease with aberrant immune activation, while insulin resistance in type 2 diabetes is increasingly thought to be associated with inflammation.8 Although hyperglycemia alone impairs the immune system, with one example being disrupted C-type lectin function,9 the immune system is weakened in many other ways.
Neutrophils, the innate immune cells that migrate to acute inflammation and eradicate extracellular pathogens, are disrupted. A 1971 study reported that the neutrophils of 31 people with diabetes had reduced migratory potential compared to people without diabetes.10 A few years later, researchers showed that all steps of neutrophil function are altered, from chemotaxis to the site of infection, adherence to the vessel wall once at the right stop, phagocytosis of the target, and bactericidal activity to finish the job.11
In 2004, neutrophils were discovered to have a new function, called NETosis, in which they produce neutrophil extracellular traps (NETs) composed of DNA armed with antimicrobial proteins. Ten years later, a Nature Medicine paper showed that this too was altered in people with diabetes. Paralleling the diabetes-as-inflammation theory, neutrophils from humans with diabetes were shown to be prone to NETosis, which impairs wound healing.12 Wound healing is also hampered by macrophages with decreased ability for efferocytosis, providing a rationale for foot ulcers becoming chronic infections.13
Other immune cells are dysregulated as well. There are fewer type 1 conventional dendritic cells and plasmacytoid dendritic cells.14 As reviewed by Daryabor and colleagues, macrophages generate foam cells, the number of type 1 innate lymphoid cells increases, and B cell-produced antibodies are glycated by hyperglycemia and activate complement less effectively.15 While this may explain the higher risk of common infections, it cannot resolve why people with diabetes are prone to malignant otitis externa.
Around nine in ten people with malignant otitis externa have diabetes, almost always caused by P aeruginosa.16 Hyperglycemia is not considered a factor in the pathogenesis, and most theories have relied on microvascular changes inhibiting immune cell trafficking.17 The minority of people with malignant otitis externa without diabetes, however, are immunocompromised for another reason: human immunodeficiency virus, transplant, or advanced cancer.18 Thus, based on the relative frequency in the population, it is possible that diabetes is acting as another immunocompromising condition for the reasons already described.
Similarly, it is not known why many of the people with rhino-orbital-cerebral mucormycosis have diabetes. One review of 929 cases of mucormycosis reported between 1940 and 2003 noted that diabetes was found in 36% of cases.19 Serum from people without diabetes inhibits rhizopus growth, whereas serum from patients with diabetic ketoacidosis stimulates growth.20
Providing final evidence that diabetes is truly an immunocompromising condition, the Emerging Risk Factors Collaboration study found a hazard ratio of 1.25 for death from cancer with diabetes.6 The increased rate was seen for cancers of the liver, pancreas, ovary, colorectum, lung, bladder, and breast. Some of these cancers are seen at higher rates in other immunocompromising conditions. Solid organ transplant predisposed to lung and liver cancer,21 HIV predisposed to lung cancer,22 and tumor necrosis factor inhibitor therapy is linked to cancers of the reproductive system and breast.23 Partially explaining the increased risk of cancer with diabetes, natural killer cells in people with diabetes are less likely to express the activating receptors NKG2D and NKp46.24 In vitro, these natural killer cells from people are less able to kill the cancer cell line K562.
To return to our attending’s question, people with diabetes are immunocompromised because of their microvascular disease in combination with aberrant immune cell function, due in part to hyperglycemic conditions. Thus, people with diabetes have more common infections, are prone to rare infections, and suffer from higher rates of cancer.
Daniel Martinez-Krams is a Class of 2026 medical student at NYU Grossman School of Medicine
Peer reviewed by Michael Tanner, MD, Executive Editor, Clinical Correlations
Image courtesy of Wikimedia Commons, source: https://commons.wikimedia.org/w/index.php?search=diabetes&title=Special:MediaSearch&go=Go&type=image
References
- Joshi N, Caputo GM, Weitekamp MR, Karchmer AW. Infections in patients with diabetes mellitus. N Engl J Med. 1999;341(25):1906-1912. doi:10.1056/NEJM199912163412507 https://pubmed.ncbi.nlm.nih.gov/10601511/
- Shah BR, Hux JE. Quantifying the risk of infectious diseases for people with diabetes. Diabetes Care. 2003;26(2):510-513. doi:10.2337/diacare.26.2.510 https://pubmed.ncbi.nlm.nih.gov/12547890/
- Abu-Ashour W, Twells LK, Valcour JE, Gamble JM. Diabetes and the occurrence of infection in primary care: a matched cohort study. BMC Infect Dis. 2018;18(1):67. doi:10.1186/s12879-018-2975-2 https://pubmed.ncbi.nlm.nih.gov/29402218/
- Carey IM, Critchley JA, DeWilde S, Harris T, Hosking FJ, Cook DG. Risk of Infection in Type 1 and Type 2 Diabetes Compared With the General Population: A Matched Cohort Study. Diabetes Care. 2018;41(3):513-521. doi:10.2337/dc17-2131 https://pubmed.ncbi.nlm.nih.gov/29330152/
- Bertoni AG, Saydah S, Brancati FL. Diabetes and the risk of infection-related mortality in the U.S. Diabetes Care. 2001;24(6):1044-1049. doi:10.2337/diacare.24.6.1044 https://pubmed.ncbi.nlm.nih.gov/11375368/
- Seshasai SRK, Kaptoge S, Thompson A, et al; Emerging Risk Factors Collaboration. Diabetes mellitus, fasting glucose, and risk of cause-specific death. N Engl J Med. 2011;364(9):829-841. doi:10.1056/NEJMoa1008862
- Atreja A, Kalra S, Rodriguez-Saldana J. Diabetes and Infection. In: Rodriguez-Saldana J, ed. The Diabetes Textbook: Clinical Principles, Patient Management and Public Health Issues. 2nd ed. Cham, Switzerland: Springer; 2023:755-785. doi:10.1007/978-3-031-25519-9_47
- Shoelson SE, Lee J, Goldfine AB. Inflammation and insulin resistance. J Clin Invest. 2006;116(7):1793-1801. doi:10.1172/JCI29069
- Ilyas R, Wallis R, Soilleux EJ, et al. High glucose disrupts oligosaccharide recognition function via competitive inhibition: A potential mechanism for immune dysregulation in diabetes mellitus. Immunobiology. 2011;216(1-2):126-131. doi:10.1016/j.imbio.2010.06.002
- Mowat AG, Baum J. Chemotaxis of polymorphonuclear leukocytes from patients with diabetes mellitus. N Engl J Med. 1971;284(12):621-627. doi:10.1056/NEJM197103252841201
- Delamaire M, Maugendre D, Moreno M, Le Goff MC, Allannic H, Genetet B. Impaired leucocyte functions in diabetic patients. Diabet Med. 1997;14(1):29-34. doi:10.1002/(SICI)1096-9136(199701)14:1<29::AID-DIA300>3.0.CO;2-V
- Wong SL, Demers M, Martinod K, et al. Diabetes primes neutrophils to undergo NETosis, which impairs wound healing. Nat Med. 2015;21(7):815-819. doi:10.1038/nm.3887
- Khanna S, Biswas S, Shang Y, et al. Macrophage dysfunction impairs resolution of inflammation in the wounds of diabetic mice. PLOS ONE. 2010;5(3):e9539. doi:10.1371/journal.pone.0009539
- Seifarth CC, Hinkmann C, Hahn EG, Lohmann T, Harsch IA. Reduced frequency of peripheral dendritic cells in type 2 diabetes. Exp Clin Endocrinol Diabetes. 2008;116(3):162-166. doi:10.1055/s-2007-990278
- Daryabor G, Atashzar MR, Kabelitz D, Meri S, Kalantar K. The Effects of Type 2 Diabetes Mellitus on Organ Metabolism and the Immune System. Front Immunol. 2020;11:1582. doi:10.3389/fimmu.2020.01582
- Grandis JR, Branstetter BF, Yu VL. The changing face of malignant (necrotising) external otitis: clinical, radiological, and anatomic correlations. Lancet Infect Dis. 2004;4(1):34-39. doi:10.1016/S1473-3099(03)00858-2
- Rubin J, Yu VL. Malignant external otitis: Insights into pathogenesis, clinical manifestations, diagnosis, and therapy. Am J Med. 1988;85(3):391-398. doi:10.1016/0002-9343(88)90592-X
- Treviño González JL, Reyes Suárez LL, Hernández de León JE. Malignant otitis externa: An updated review. Am J Otolaryngol. 2021;42(2):102894. doi:10.1016/j.amjoto.2020.102894
- Roden MM, Zaoutis TE, Buchanan WL, et al. Epidemiology and outcome of zygomycosis: a review of 929 reported cases. Clin Infect Dis. 2005;41(5):634-653. doi:10.1086/432579
- Ferguson BJ. Mucormycosis of the nose and paranasal sinuses. Otolaryngol Clin North Am. 2000;33(2):349-365. doi:10.1016/S0030-6665(00)80010-9
- Engels EA, Preiksaitis J, Zingone A, Landgren O. Circulating antibody free light chains and risk of posttransplant lymphoproliferative disorder. Am J Transplant. 2012;12(5):1268-1274. doi:10.1111/j.1600-6143.2011.03954.x
- Silverberg MJ, Lau B, Achenbach CJ, et al. Cumulative Incidence of Cancer among HIV-infected Individuals in North America. Ann Intern Med. 2015;163(7):507-518. doi:10.7326/M14-2768
- Ilham S, Willis C, Kim K, et al. Cancer incidence in immunocompromised patients: a single-center cohort study. BMC Cancer. 2023;23(1):33. doi:10.1186/s12885-022-10497-4
- Berrou J, Fougeray S, Venot M, et al. Natural killer cell function, an important target for infection and tumor protection, is impaired in type 2 diabetes. PLOS ONE. 2013;8(4):e62418. doi:10.1371/journal.pone.0062418