Peer Reviewed
As a medical student and researcher, I am fascinated by the mechanisms of evolution in human disease. I am particularly intrigued by oncology, where evolution unfolds in real-time. Somatic cells acquire mutations as we age, allowing for clonal proliferation and tumorigenesis within years to decades. Current computational oncology research uses genomic sequencing as a magnifying glass to identify those initial insults to the tissue‘s genome that permit clonal selection.1-3 It remains unclear which biological processes and environmental exposures linked to cancer allow for the acquisition of de novo mutations (thought of as “mutagens”, such as tobacco carcinogens,4 ultraviolet light, and oncogenic viruses) and which alter the tissue microenvironment to allow for the unrestrained clonal expansion of premalignant cells (considered an alternate hypothesis to carcinogenesis).5,6 Untangling the root mechanisms of why patients get cancer can identify high-risk patient populations and aid in the development of novel screening methods, both of which are at the forefront of preventive medicine.
Complications of a faulty immune system
Patient A: A 41-year-old man presents with red lesions on the nasal skin, oral mucosa, and lower extremities. The patient was diagnosed with HIV 15 years ago and was intermittently taking antiretrovirals, although lost to follow-up in 2020. Three months ago, he noticed a dark red lesion in his mouth, which led to two of his teeth falling out. He was seen in a clinic and was found to have an HIV viral load of 20,000 copies/mL, a CD4 count of 37, and a platelet count of 41,000. He began taking Biktarvy but refused a biopsy of the oral lesion. Over the past few months, new lesions appeared over his nose and lower extremities, and he developed diffuse lymphadenopathy and lower extremity swelling. He also complains of persistent congestion and fatigue but denies weight loss, fever, and night sweats.
Patient B: A 58-year-old woman presents with abdominal pain, fatigue, and unintentional weight loss. The patient underwent a kidney transplant six years ago for end-stage renal disease secondary to autosomal dominant polycystic kidney disease. She has been on maintenance immunosuppression with tacrolimus, mycophenolate mofetil, and prednisone. Over the past two months, she experienced vague abdominal discomfort, spotty blood in her stool, and progressive weight loss of 20 pounds. She also reports progressive fatigue but denies vomiting or changes in bowel habits.
These two vignettes represent patients I cared for on my internal medicine rotation, whom I was working up for suspected malignancies. They presented at different hospitals with different cancers, environmental exposures, socioeconomic status, racial and ethnic groups, and genetic and lifestyle risk factors. However, while caring for them, one aspect of their history united their stories for me: cancer in the setting of immune dysfunction and dysregulation.
The immune system has long been considered essential for preventing the development of tumors. Three primary roles have been established for this function:7 first, the immune system eliminates pathogens and inhibits tissue inflammation, which can be tumorigenic when left unregulated. Secondly, the immune system protects the host from virus-induced tumors by suppressing viral infections. Third is the concept of “tumor immune surveillance,” where the immune system can identify and eliminate cancerous or precancerous cells based on the presence of tumor-specific molecules.8 This concept was first put forth by Burnet in 1957: “If the concept of immunological surveillance is legitimate…conditions associated with depression of the immune system, whether genetic, induced by drugs, or of other origin should increase the likelihood of cancer.”9
Cancer incidence and tumorigenesis in HIV-infected patients
Patient A was diagnosed with Kaposi’s sarcoma, a vascular malignancy caused by oncogenic viral integration of human herpesvirus 8 (HHV8, a well-described mutagen).9 Kaposi’s sarcoma is grouped into distinct epidemiological forms affecting elderly men of Mediterranean or Ashkenazi ancestry, populations endemic to Central and Eastern Africa, and patients with acquired immunodeficiency syndrome (AIDS).10-12 With clinical signs of immunosuppression evidenced by his low CD4 T cell count, his immune system was unable to suppress the HHV8 infection. Key viral proteins such as latency-associated nuclear antigen inhibit tumor suppressor pathways, including p53 and Rb, while viral G-protein-coupled receptors and cytokines activate signaling pathways like PI3K/AKT and MAPK, promoting cell survival, proliferation, and angiogenesis.11
As a result of the AIDS pandemic, Kaposi’s sarcoma became one of the most common cancers affecting men and children infected with HIV. Prior to the introduction of highly active antiretroviral therapy, up to one-third of HIV-infected gay men had evidence of Kaposi’s sarcoma, compared to 1 in 100,000 in the general population.10 I treated a 75-year-old gay man in Ambulatory Care Clinic for his yearly wellness visit. He moved to Greenwich Village from Brooklyn in the 1970s and worked as a waiter for 30 years, mainly in restaurants owned by older gay men. By the mid-1990s, all of the restaurants had closed; only one of his friends from his thirties and forties are still alive today, largely due to Kaposi’s sarcoma. I didn’t think I would make it ’til fifty… I was going to three funerals a week, he reflected. Other AIDS-related malignancies that have been well characterized include cervical and non-Hodgkin’s lymphoma, due to unregulated infections of human papillomavirus and Epstein-Barr virus, respectively.13 Tumors unrelated to viral infections, such as colorectal, kidney, melanoma, and breast cancer, do not have the same increased risk.
Tumor surveillance hypothesis, from mice to people
The role of the immune system in regulating oncogenic viral replication is well-described and widely accepted. However, the tumor immune surveillance hypothesis is more convoluted, largely due to poor causational evidence.8 The earliest experiments tested whether mice with an impaired immune system would exhibit an increased incidence of spontaneous or chemically induced tumors. This was studied by removing the thymus of neonatal mice, dosing with anti-lymphocyte pharmacotherapies, or genetically altering lymphocyte receptors, with discordant results. The strongest evidence came about with the discovery of gammadelta T cells. By selectively depleting gammadelta T cells and exposing mice to various environmental chemicals, mice exhibited a higher incidence of sarcomas and skin tumors compared to wild-type controls.14
Epidemiological studies have corroborated these findings. Engels and colleagues landscaped cancer risk in solid organ transplant patients15 who are on chronic immunosuppressive medications to prevent rejection of organ transplants. The study included 175,732 transplant recipients from 1987 to 2008, encompassing 58% kidney, 22% liver, 10% heart, and 4% lung transplant patients. The authors noted an increased risk of 32 different malignancies in organ transplant patients compared to the general population, including malignancies caused by viral infection (non-Hodgkin’s lymphoma, Kaposi’s sarcoma, and cancers of the liver, oropharynx, anus, vulva, and penis) and non-infection related cancers (lung, kidney, colorectal, thyroid, bladder, melanoma, among others).15
Patient B, with a history of end-stage renal disease and kidney transplant on long-term immunosuppressive medications, went on to be diagnosed with stomach cancer. Her increase in cancer risk is multifactorial and could be attributed to (1) end-stage organ dysfunction, (2) surveillance bias, (3) direct mutagenic effects of medications, or (4) dysfunctional tumor immune surveillance. However, an earlier study of Australian kidney transplant patients found that cancer risk was significantly increased after transplantation and drug-induced immunosuppression, with only a mild increase in cancer risk for end-stage renal patients on dialysis.16,17 There is some evidence that specific medications used in immunosuppressed patients can have direct mutagenic effects. Antiviral treatment (ganciclovir for Cytomegalovirus infections) after bone marrow transplant can induce C>A transversion mutations. These same mutations were identified in patients with clonal hematopoiesis and acute myeloid leukemia after bone marrow transplant.18 Azathioprine (which acts as a purine analog to inhibit DNA replication in rapidly dividing lymphocytes) was found to cause C>T transition mutations in a subset of squamous cell carcinoma samples from patients treated with various cocktails of immunosuppressants.19 While concerning, the increase in cancer risk cannot be explained by medication-induced somatic mutagenesis alone. Patients with primary immunodeficiencies similarly have an increase in cancer risk, with studies reporting a 1.4- to 2.3-fold increase,18,20 highlighting the essential role of a functional immune system. The most plausible hypothesis for the increased cancer risk is likely a combination of mutagenic effects of immunosuppressant medications, and loss of immune surveillance in eliminating premalignant transformed cells.15
Future research directions
If true, the tumor immune surveillance hypothesis would suggest that patients with chronic immunosuppression would have higher rates of somatic mutations, probably in well-known cancer driver genes. This hypothesis is difficult to test due to the challenges posed by sequencing somatic tissues. However, a novel sequencing method was recently published that allows for whole-exome and targeted gene sequencing with an error rate of <5 bases per billion base pairs, allowing for acute somatic mutation rates.21 These results would clarify this decades-long and highly debated hypothesis toward understanding why high-risk immunosuppressed patients exhibit a higher incidence of cancer burden.
Future clinical research should also prioritize the development and refinement of cancer screening protocols specifically tailored for immunocompromised populations. Given the heightened risk and unique cancer epidemiology in these patients, traditional screening guidelines may not be sufficient. Studies should aim to identify biomarkers and imaging techniques that are more sensitive and specific to early-stage cancers in immunocompromised individuals. For example, liquid biopsy technologies that measure rates of somatic mutagenesis (in blood or other easily accessible tissues) could offer a noninvasive and highly sensitive screening tool. Additionally, research should explore the optimal frequency and combination of screening modalities to balance early detection with the potential risks and costs associated with increased surveillance. By customizing screening strategies to the unique needs of immunocompromised patients, we can improve early detection rates, enable timely intervention, and ultimately enhance survival outcomes in this vulnerable population.
By Jacob Rozowsky is a Class of 2027 medical student at NYU Grossman School of Medicine
Reviewed by Michael Tanner, MD, Executive Editor, Clinical Correlations
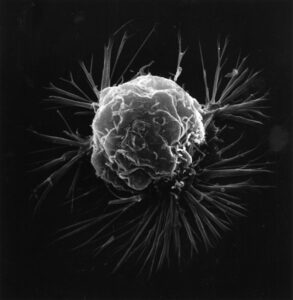
Image courtesy of Wikimedia Commons, source: Unknown photographer, Public domain, via https://commons.wikimedia.org/wiki/File:Breast_cancer_cell_(2).jpg
References
- Alexandrov LB, Nik-Zainal S, Wedge DC, et al. Signatures of mutational processes in human cancer. Nature. 2013;500(7463):415-421. doi:10.1038/nature12477 https://www.nature.com/articles/nature12477
- Alexandrov LB, Nik-Zainal S, Wedge DC, Campbell PJ, Stratton MR. Deciphering Signatures of Mutational Processes Operative in Human Cancer. Cell Rep. 2013;3(1):246-259. doi:10.1016/j.celrep.2012.12.008
- Alexandrov LB, Kim J, Haradhvala NJ, et al. The repertoire of mutational signatures in human cancer. Nature. 2020;578(7793):94-101. doi:10.1038/s41586-020-1943-3 https://www.nature.com/articles/s41586-020-1943-3
- Alexandrov LB, Ju YS, Haase K, et al. Mutational signatures associated with tobacco smoking in human cancer. Science. 2016;354(6312):618-622. doi:10.1126/science.aag0299
- Riva L, Pandiri AR, Li YR, et al. The mutational signature profile of known and suspected human carcinogens in mice. Nat Genet. 2020;52(11):1189-1197. doi:10.1038/s41588-020-0692-4
- Lopez-Bigas N, Gonzalez-Perez A. Are carcinogens direct mutagens? Nat Genet. 2020;52(11):1137-1138. doi:10.1038/s41588-020-00730-w https://pubmed.ncbi.nlm.nih.gov/33128047/
- Swann JB, Smyth MJ. Immune surveillance of tumors. J Clin Invest. 2007;117(5):1137-1146. doi:10.1172/JCI31405
- Dunn GP, Bruce AT, Ikeda H, Old LJ, Schreiber RD. Cancer immunoediting: from immunosurveillance to tumor escape. Nat Immunol. 2002;3(11):991-998. doi:10.1038/ni1102-991
- Chang Y, Cesarman E, Pessin MS, et al. Identification of Herpesvirus-Like DNA Sequences in AIDS-Associated Kaposi’s Sarcoma. Science. 1994;266(5192):1865-1869. doi:10.1126/science.7997879
- Beral V, Peterman TA, Berkelman RL, Jaffe HW. Kaposi’s sarcoma among persons with AIDS: a sexually transmitted infection? Lancet. 1990;335(8682):123-128. doi:10.1016/0140-6736(90)90001-l https://pubmed.ncbi.nlm.nih.gov/1967430/
- Mesri EA, Cesarman E, Boshoff C. Kaposi’s sarcoma and its associated herpesvirus. Nat Rev Cancer. 2010;10(10):707-719. doi:10.1038/nrc2888
- Cesarman E, Damania B, Krown SE, Martin J, Bower M, Whitby D. Kaposi sarcoma. Nat Rev Dis Primers. 2019;5(1):9. doi:10.1038/s41572-019-0060-9
- Grulich AE, van Leeuwen MT, Falster MO, Vajdic CM. Incidence of cancers in people with HIV/AIDS compared with immunosuppressed transplant recipients: a meta-analysis. Lancet. 2007;370(9581):59-67. doi: 10.1016/S0140-6736(07)61050-2.
- Girardi M, Oppenheim DE, Steele CR, et al. Regulation of Cutaneous Malignancy by Gammadelta T Cells. Science. 2001;294(5542):605-609. doi:10.1126/science.1063916
- Engels EA, Pfeiffer RM, Fraumeni JF Jr, et al. Spectrum of Cancer Risk Among US Solid Organ Transplant Recipients. JAMA. 2011;306(17):1891-901. doi: 10.1001/jama.2011.1592.
- Vajdic CM, McDonald SP, McCredie MRE, et al. Cancer Incidence Before and After Kidney Transplantation. JAMA. 2006;296(23):2823-31. doi: 10.1001/jama.296.23.2823.
- Engels EA. Epidemiologic perspectives on immunosuppressed populations and the immunosurveillance and immunocontainment of cancer. Am J Transplant. 2019;19(12):3223-3232. doi:10.1111/ajt.15495
- De Kanter JK, Peci F, Bertrums E, et al. Antiviral treatment causes a unique mutational signature in cancers of transplantation recipients. Cell Stem Cell. 2021;28(10):1726-1739.e6. doi:10.1016/j.stem.2021.07.012
- Moody S, Senkin S, Islam SMA, et al. Mutational signatures in esophageal squamous cell carcinoma from eight countries with varying incidence. Nat Genet. 2021;53(11):1553-1563. doi:10.1038/s41588-021-00928-6
- Jonkman-Berk BM, Van Den Berg JM, Ten Berge IJM, et al. Primary immunodeficiencies in the Netherlands: national patient data demonstrate the increased risk of malignancy. Clin Immunol. 2015;156(2):154-162. doi:10.1016/j.clim.2014.10.003
- Lawson ARJ, Abascal F, Nicola PA, et al. Somatic mutation and selection at epidemiological scale. medRxiv. Published online November 1, 2024. doi:10.1101/2024.10.30.24316422