Edited by Tania Ahuja, Pharm.D., BCPS
Faculty peer reviewed
Bronchiectasis is an uncommon condition that is characterized by irreversible dilation of the bronchi. Chronic pulmonary infections and airway inflammation cause bronchial damage through destruction of the muscular and elastic layer of the bronchial wall leading to bronchiectasis. Bronchiectasis is associated with serious pulmonary infections, inflammation, chronic cough, and increased sputum production secondary to pooling in the dilated tubules. On physical exam patients can present with rhonchi, crackles, wheezing, or clubbing. High-resolution CT scanning of the chest is considered the gold standard for diagnosis. 1,2,3,4
The goals of therapy include improving symptoms of cough and mucociliary clearance, enhancing bronchodilation, preventing progression of further airway damage, and reducing the number of exacerbations. There is limited data on the treatment of idiopathic bronchiectasis, however prolonged antimicrobial therapy is often warranted to prevent worsening infections. Antimicrobial therapy should be initiated in patients experiencing an acute exacerbation after sputum cultures are obtained to better help guide therapy. In a study by O’Donnel et al, patients with bronchiectasis were considered to have an acute exacerbation if they had 4 or more of the following symptoms: change in sputum production, increased dyspnea, increased cough, fever (>38 ºC), increased wheezing, fatigue or malaise, reduced pulmonary function, evidence of radiographic or auscultatory changes.5
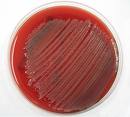
Antimicrobial therapy should target the following common pathogens depending on the patient specific risk factors: Haemophilus influenza, Pseudomonas aeruginosa, Staphylococcus aureus, and Streptococcus pneumoniae. 1-3. Patients with cystic fibrosis, severe chronic obstructive pulmonary disease or recent antibiotic use are at greater risk for P. aeruginosa.4,6  Other patient populations at risk for P. aeruginosa include: immunocompromised patients such as those on chronic oral steroids or with malignancy, asplenic patients,  patients with renal or liver disease and chronic heart failure.7 In cystic fibrosis (CF), P. aeruginosa infections have shown to cause deterioration of pulmonary function, respiratory failure, and death. P. aeruginosa usually becomes a chronic infection and is rarely eradicated, despite the use of intravenous antibiotic therapy. There is little data in non-CF patients on the long term outcomes when treating             P. aeruginosa.
Once a patient with bronchiectasis is thought to have an acute exacerbation, sputum cultures should be obtained prior to antimicrobial therapy. Once sputum microbiology results are available de-escalation of antimicrobial therapy is essential to prevent future resistance.1 Fluoroquinolones such as ciprofloxacin or levofloxacin are reasonable outpatient antibiotics in patients with severe symptoms for 7-14 days. 1,2,4,8,9 However it is essential to evaluate a patient’s prior antimicrobial therapy and culture and sensitivity data in order to prevent inappropriate treatment or future resistance. Prior fluoroquinolone use is a risk factor for subsequent infection with quinolone-resistant extended spectrum beta lactamase (ESBL)-producing organisms, and there is also a potential connection with colonization or infection with methicillin-resistant Staphylococcus aureus (MRSA).10
Inhalation antimicrobial therapy, such as inhaled tobramycin can also be considered for the management of an acute exacerbation. However, inhalation therapy often results in prolonged duration of therapy leading to resistance and unwarranted side effects such as wheezing. In addition, although treatment in non-CF patients with inhaled tobramycin has been reported to decrease pseudomonas density; there is no improvement in quality of life, decreased need for additional antibiotics, or improvement in pulmonary function. 11-14 A study by Barker et al, looked at the use of tobramycin solution 300mg for inhalation in 37 non-CF bronchiectasis for 6 weeks and showed to have significant improvement in medical condition (62% vs. 38% in placebo) and 35% eradication of P. aeruginosa compared to none in placebo. Tobramycin resistance developed in 11% of patients treated with tobramycin and 3% of patients treated with placebo. The mean change in FEV1 did not vary between the two groups and patients in the tobramycin group experienced significant side effects such as cough, dyspnea, wheezing, and noncardiac chest pain, limiting their compliance.15 Finally, Bilton et al, looked at tobramycin inhalation solution added to oral ciprofloxacin therapy for the treatment of acute exacerbation of bronchiectasis due to P.aeruginosa. The combination group showed an improved microbiological outcome but patients experienced increased frequency of wheezing. 12
In patients that are hospitalized with more severe symptoms and risk factors for resistant organisms, treatment with intravenous antimicrobials is often warranted. It is important to use antimicrobials with activity against P. aeruginosa and be cognizant of the fact that most of these patients may have been treated as an outpatient with a fluoroquinolone leading to the selection of drug-resistant organisms and the unwanted development of colonization with a multidrug-resistant organism. Antipseudomonal beta lactams, carbapenems, or aminoglycosides may be considered as treatment options for acute exacerbations in these patients.16,7
Tsang et al, studied the efficacy of oral levofloxacin as compared to intravenous ceftazidime for 10 days in 35 patients for the empiric treatment of acute exacerbations of bronchiectasis. There was no significant difference between the two groups and both groups had improvement in sputum volume, sputum purulence score, dyspnea, and cough score.8 Rayner et al, assessed the safety and efficacy of long term ciprofloxacin, defined as treatment for 90 days in the management of severe bronchiectasis in 10 patients. Ciprofloxacin was well tolerated and patients had a significant improvement in the number of exacerbations and symptoms, however antimicrobial resistance developed in 2 out of 10 patients to P. aeruginosa.9
Fluoroquinolone resistance to P. aeruginosa is an emerging concern today and it is therefore crucial to be sensitive to the resistance patterns within your institution and geographical area. At NYU Langone Medical Center, only 63% of non-ICU P. aeruginosa isolates were found susceptible to ciprofloxacin and only 51% of ICU isolates were susceptible in 2008. Consequently, careful antimicrobial selection is warranted in hospitalized patients who require coverage against P. aeruginosa to prevent treatment failure. When a non-CF patient experiences an acute exacerbation, empiric treatment for P. aeruginosa should be initiated only if the patient meets specific risk factors for P. aeruginosa. If empiric treatment for P. aeruginosa is determined to be appropriate, it is imperative that clinicians become familiar with their local institution’s P. aeruginosa susceptibility patterns and choose antimicrobials with greater than 50-60% susceptibility to prevent treatment failure. In addition, this will help prevent the selection of drug-resistant organisms, infections with multidrug-resistant organisms, or super-infections like Clostridium difficile.
Commentary by Neal Steigbigel MD, Professor, NYUÂ Division of Infectious Diseases/Immunology
In considering this well-written article on the treatment of brochiectasis complicated by infection with Pseuodomonas aeruginosa, consider the as yet unproven potential role of macrolides, especially azithromycin, used for several months, in patients with chronic lung disease/bronchiectasis, especially if they are heavily colonized with P.aeruginosa.
The suggestion originally comes from older studies in Japan demonstrating the major benefits of macrolides, originally demonstrated with erythromycin, in patients in that country with “diffuse panbronchiolitis” (a potentially fatal lung condition in some individuals esp in Japan, possibly of genetic origin). That finding led Japanese scientists to their discoveries of the multiple potent anti-inflammatory effects of the macrolides and later to the demonstration of potent effects of macrolides in down-regulating some P. aeruginosa virulence factors, including adhesins for host cells. Those effects are demonstrated even though the macrolides have no traditional antibiotic (killing or growth inhibiting effects) on that organism. More recently several studies in patients with cystic fibrosis (CF), who are often heavily colonized with that organism, have demonstrated significant improvements in pulmonary function when they are treated for months with azithromycin. Azithromycin is now subject to great interest in treatment of COPD; a large NIH-sponsored controlled trial is now underway. These aspects of the macrolides with literature citations can be found in the most recently revised chapter on the macrolides by Sumathi Sivapalasingam and me in latest edition of “Principles and Practice of Infectious Diseases” ed by Mandell, Bennett and Dolin, Churchill-Livingstone-Elsevier, 2010 (actually already available this year).
References
1. O’Donnell, A. E. Â Bronchiectasis. Chest 2008:134;815-823
2. Barker AF. Bronchiectasis. NEJM 2002;346(18):1383-93.
3. Emmons EE. Bronchiectasis from WebMD. 1996-2008. Available online. http://emedicine.medscape.com/article/296961-overview. Accessed July 30th, 2009
4. Rosen MJ. Chronic cough due to bronchiectasis: ACCP evidence-based clinical practice guidelines. Chest 2006;129(suppl):122S-131S
5. O’Donnell AE, Barker AF, Ilowite JS, Fick RB. Treatment of idiopathic bronchiectasis with aerosolized recombinant human DNase I. Chest 1998;113:1329-34.
 6. Davies G, Wells A.U., et al. The effect of Pseudomonas aeruginosa on pulmonary function in patients with bronchiectasis. Eur Respir J 2006;28:974-979
7. Mandell LAÂ et al: Infectious Diseases Society of America/American Thoracic Society consensus guidelines on the management of community-acquired pneumonia. Clin Infect Dis 2007;44(Suppl 2):S27
8. Tsang KW, Chan W-M, Ho P-L, et al. A comparative study on the efficacy of levofloxacin and ceftazidime in acute exacerbations of bronchiectasis. Eur Respir J 1999; 14:1206-1209
9. Rayner CF, Tillotson G, Cole PJ, et al. Efficacy and safety of long-term ciprofloxacin in the management of severe bronchiectasis. J Antimicrob Chemother 1994;34:149-156
 10. Paterson DL. “Collateral Damage” from Cephalosporin or Quinolone Antibiotic Therapy. Clin Infect Dis 2004; 38(Suppl 4): S341-5.
11. Drobnic ME et al. Inhaled tobramycin in non-cystic fibrosis patients with bronchiectasis and chronic bronchial infections with Pseudomonas aeruginosa. Ann Pharmacotherapy 2005;39:39-44
12. Rubin BK, Eng M. Aerosolized Antiobiotics for Non-Cystic Fibrosis Bronchiectasis. J of Aer Med and Pulm Drug Deliv 2008;21:71-76
13. Bilton D, Henig N, Morrissey B, Gotfried M. Addition of Inhaled Tobramycin to Ciprofloxacin for Acute Exacerbations of Pseudomonas aeruginosa Infections in Adult Bronchiectasis. Chest 2006;130:1503-1510
14. Scheinberg P, Shore E. A pilot study of the efficacy and safety of tobramycin solution for inhalation in patients with severe bronchiectasis. Chest 2005;127:1420-1426
15. Barker AF, Couch L, Fiel SB, et al. Tobramycin solution for inhalation reduces sputum Pseudomonas aeruginosa density in bronchiectasis. Am J Respir Crit Care Med 2000; 162:481-485
16. Murray MP et al. Â Assessing response to treatment of exacerbation of bronchiectasis in adults. Eur Respir J 2009:33:312-317
 Â

One comment on “Antimicrobial Therapy Geared at Pseudomonas aeruginosa for Bronchiectasis”
Comments are closed.