Faculty Peer Reviewed
“Red Meat Kills.†“Red Meat a Ticket to Early Grave.†“A Hot Dog a Day Raises Risk of Dying.†Such were the headlines circulating in popular press last year when the Annals of Internal Medicine released details of an upcoming article out of Frank Hu’s research group at the Harvard School of Public Health [1-3]. Analyzing long-term prospective data from two large cohort studies, researchers found that individuals who ate a serving of unprocessed red meat each day had a 13% higher risk of mortality during the study period. The numbers were even more grim for processed meats, as a one-serving-per-day increase in such foods as bacon or hot dogs was associated with a 20% increase in mortality risk. Hu and colleagues ultimately concluded that 9.3% of the observed deaths in men and 7.6% of the deaths in women could have been avoided by participants consuming less than 0.5 daily servings (42 g) of red meat [4].
While this study received a great deal of media buzz, it is merely the latest in a long line of studies over the past decade that have tried to better understand how red meat consumption may impact the development of chronic disease. Indeed, our own research group recently set out to answer that same question, although through a different approach: focusing on dietary patterns rather than specific diet elements. Compared to the “single nutrient†or “single food†approach, this analytic method more fully accounts for biochemical interactions between nutrients, as well as interrelationships between dietary components that cause difficulty in distinguishing individual food or nutrient effects. We followed over 11,000 individuals in Bangladesh for nearly 7 years, identifying distinct dietary patterns as well as the associations between these patterns and risk of adverse cardiovascular outcomes. In short, we found that adherence to an animal protein diet increased risk of death from overall cardiovascular disease, especially heart disease. In fact, after stratifying adherence to the animal protein diet into 4 levels, the most adherent group had twice the risk of heart disease mortality compared to the least adherent. While striking, these results inevitably raise the question of what role red meat in particular played in increased mortality, as it was only a component of the more unhealthy diet [5].
The contrasting analytical approaches in these two studies highlight the difficulty in fully understanding how red meat may affect cardiovascular health and mortality. It is believed that adverse outcomes from red meat intake are mediated mainly through the effects of high saturated fat on blood low-density lipoprotein and other cholesterol levels, although high sodium content in processed red meat may also play a role by elevating blood pressure and impairing vascular compliance. Additionally, nitrate preservatives, which are used in processed meats, have been shown in experimental models to reduce insulin secretion, impair glucose tolerance, and promote atherosclerosis [6].
Although multiple studies have shown an association between red meat and cardiovascular disease [7-10], the magnitude of risk is somewhat debatable. In a recent set of meta-analyses, for example, one found equivocal evidence for the influence of meat on cardiovascular disease [11], while another showed consumption of processed red meat, but not unprocessed red meat, to be associated with risk of coronary heart disease [6]. Much of this cloudiness is likely due to inconsistencies across studies in terms of study design, as well as how each defines meat intake and meat types (distinguishing what constitutes “red,†“processed,†or “leanâ€). Taking all of this into consideration, the best current evidence still seems to indicate that red meat consumption at very high levels conveys increased risk of cardiovascular disease, with processed meats likely increasing that risk. This is similar to what has been observed with respect to type 2 diabetes and colon cancer, as red meat (particularly processed meats) has been linked to a higher risk of both [12-15].
A more complete understanding of healthy eating and advisable intake of red meat is truly of vital importance. Although cardiovascular disease remains the world’s leading cause of death, it has been posited that over 90% of cases may be preventable simply by modifying diet and lifestyle [16-18]. A recent literature review summarized foods that are protective against cardiovascular disease: vegetables, nuts, and monounsaturated fats, as well as Mediterranean, prudent, and high-quality diets [11]. Conversely, as discussed above, current evidence indicates most convincingly that high intake of processed red meats, particularly as part of a Western diet, carries significant risk for increased mortality and adverse cardiovascular outcomes. Many questions, though, remain unanswered–namely, to what extent unprocessed red meat can be grouped with its processed counterpart in terms of health risks, as well as what risk reduction may be possible by substituting lean red meats for either processed or unprocessed meat (which has not yet been addressed in any large prospective study) [19].
Without a full understanding of red meat’s health effects, clinicians are faced with the need to settle for the best available evidence to counsel their patients in need of dietary guidance. The 2010 US Dietary Guidelines for Americans advise for moderation of red meat intake, mainly due to the expected effect of its saturated fat and cholesterol on blood cholesterol [20]. However, with unprocessed and processed red meats having similar levels of saturated fat yet distinctly different clinical outcomes, current dietary recommendations on meat consumption are shown to be based almost solely on the “avoidance of fat†postulate. The resultant dietary recommendations, neither comprehensive nor specific, are justifiably limited by our current level of understanding. Without elucidating the health effects of preservatives in processed meats or potential risk reduction from substitution of lean meats for standard red meat, it is nearly impossible to make more nuanced or quantitative recommendations.
So how does all of this impact the day-to-day practice of a clinician–particularly one in primary care? There will likely never come a day when it is realistic to counsel or expect every patient to avoid red meat completely. In light of recent evidence, though, it is certainly justifiable to recommend moderation, particularly with respect to processed types. Until further research is able to establish hard-and-fast guidelines, qualitative guidance will remain the best evidence-based advice that physicians can hand down. In other words, if a patient’s going to have a cow (or lamb or pork, for that matter), emphasize moderation and recommend that it not be processed.
Tyler R. McClintock is an M.D./M.S. candidate in the Department of Environmental Medicine at New York University School of Medicine. Under the direction of Dr. Yu Chen, his research focuses on how environmental and dietary factors are related to the risk of chronic diseases.
Tyler R. McClintock is a 4th year medical student at NYU School of Medicine
Peer reviewed by Michelle McMacken, MD, Dept. of Medicine (GIM Div.) NYU Langone Medical center
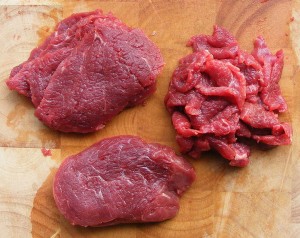
Image courtesy of Wikimedia Commons
References
1. Wanjek C. Red meat a ticket to early grave, Harvard says. Yahoo! Daily News. March 12, 2012. http://article.wn.com/view/2012/03/12/Red_Meat_a_Ticket_to_Early_Grave_Harvard_Says/#/related_news. Accessed May 23, 2012.
2. Dale R. Red meat ‘kills.’ The Sun. March 13, 2012.
3. Ostrow N. A hot dog a day raises risk of dying, Harvard study finds. Bloomberg Businessweek. March 12, 2012. http://www.businessweek.com/news/2012-03-12/a-hot-dog-a-day-raises-risk-of-dying-harvard-study-finds. Â Accessed March 23, 2012.
4. Pan A, Sun Q, Bernstein AM, et al. Red meat consumption and mortality: results from 2 prospective cohort studies. Arch Intern Med. 2012;172(7):555-63.
5. Chen Y, McClintock TR, Segers S, et al., Prospective investigation of major dietary patterns and risk of cardiovascular mortality in Bangladesh. Int J Cardiol. 2012 May 3. [Epub ahead of print]
6. Micha R, Wallace SK, Mozaffarian D. Red and processed meat consumption and risk of incident coronary heart disease, stroke, and diabetes mellitus: a systematic review and meta-analysis. Circulation. 2010;121(21):2271-2283.
7. Fraser GE. Associations between diet and cancer, ischemic heart disease, and all-cause mortality in non-Hispanic white California Seventh-day Adventists. Am J Clin Nutr. 1999;70(3 Suppl):532S-538S.
8. Sinha R, Cross AJ, Graubard BI, Leitzmann MF, Schatzkin A. Meat intake and mortality: a prospective study of over half a million people. Arch Intern Med, 2009;169(6):562-571. http://www.ncbi.nlm.nih.gov/pubmed/19307518
9. Kelemen LE, Kushi LH, Jacobs DR Jr, Cerhan JR. Associations of dietary protein with disease and mortality in a prospective study of postmenopausal women. Am J Epidemiol. 2005;161(3):239-249.
10. Kontogianni MD, Panagiotakos DB, Pitsavos C, Chrysohoou C, Stefanidis C. Relationship between meat intake and the development of acute coronary syndromes: the CARDIO2000 case-control study. Eur J Clin Nutr. 2008;62(2):171-177.
11. Mente A, deKoning L, Shannon HS, Anand SS. A systematic review of the evidence supporting a causal link between dietary factors and coronary heart disease. Arch Intern Med. 2009;169(7):659-669. http://www.ncbi.nlm.nih.gov/pubmed/19364995
12. McAfee AJ, McSorley EM, Cuskelly GJ, et al. Red meat consumption: an overview of the risks and benefits. Meat Sci. 2010;84(1):1-13. http://www.ncbi.nlm.nih.gov/pubmed/20374748
13. Fung TT, Schulze M, Manson JE, Willett WC, Hu FB. Dietary patterns, meat intake, and the risk of type 2 diabetes in women. Arch Intern Med. 2004;164(20):2235-2240.
14. Pan A, Sun Q, Bernstein AM, et al. Red meat consumption and risk of type 2 diabetes: 3 cohorts of US adults and an updated meta-analysis. Am J Clin Nutr. 2011;94(4):1088-1096.
15. Larsson SC, Wolk A. Meat consumption and risk of colorectal cancer: a meta-analysis of prospective studies. Int J Cancer. 200;119(11):2657-2664.
16. Lopez AD, Mathers CD. Measuring the global burden of disease and epidemiological transitions: 2002-2030. Ann Trop Med Parasitol. 2006;100(5-6):481-499.
17. Yusuf S, Reddy S, Ounpuu S, Anand S. Global burden of cardiovascular diseases: part I: general considerations, the epidemiologic transition, risk factors, and impact of urbanization. Circulation. 2001;104(22):2746-2753.
18. Ornish D. Dean Ornish on the world’s killer diet. TED Talk. Monterey, CA. February, 2006.
19. Roussell MA, Hill AM, Gaugler TL, et al. Beef in an Optimal Lean Diet study: effects on lipids, lipoproteins, and apolipoproteins. Am J Clin Nutr. 2012;95(1):9-16. http://www.unboundmedicine.com/washingtonmanual/ub/citation/22170364/Beef_in_an_Optimal_Lean_Diet_study:_effects_on_lipids_lipoproteins_and_apolipoproteins_
20. U.S. Department of Agriculture and U.S. Department of Health and Human Services. Dietary Guidelines for Americans, 2010. 7th Edition, Washington, DC: U.S. Government Printing Office, December 2010. Page 1 of 4. http://health.gov/dietaryguidelines/dga2010/dietaryguidelines2010.pdf

One comment on “Have a Cow? How Recent Studies on Red Meat Consumption Apply to Clinical Practice”
I read with great interest Mr McClintock’s very well-done piece on red meat and cardiac risk. In fact, this has been a hotly discussed topic where I practice, due to both the cited cohort analyses and some basic research results (Nature Medicine (2013) doi:10.1038/nm.3145). To study human nutrition and its consequences to health is an extremely complex job, and Mr McClintock wisely concludes with recommendations for moderation, rather than a complete avoidance of red meat.
I want to point a few studies that I think can enrich the discussion. In the third paragraph the author reasons that high saturated fat and sodium content could explain negative health effects of red meat. There was a recent update to a Cochrane analysis on saturated fat (Hooper et al, Cochrane Database Syst Rev. 2012 May 16;5:CD002137. doi: 10.1002/14651858.CD002137.pub3). The researchers pooled results from randomized controlled clinical trials and found no association between reduction of saturated fat intake and mortality among 71,790 subjects. Indeed, there was a relative reduction of cardiac events of 14%, especially in the subgroup of men who were followed the longest. These are results from clinical trials, stronger than cohort or epidemiological studies. On my side, I feel uneasy with the NNT for mortality: infinite (or at least more than 72 thousand – it is unlikely that I will save a single person’s life during my whole career by recommending against red meat). What about the “French paradox� Professor Ferrières, in an article published in 2004 (Heart 90:107-11) found that there isn’t a French paradox, but rather a pan-European paradox – he drew a regression line showing a clear linear relationship between saturated fat intake and heart disease, just upside down (the more saturated fat, the less heart disease among studied countries in Europe). Even more recently, reanalysis of data from an old Australian clinical trial studying 458 men (BMJ 2013;346:e8707 doi: 10.1136/bmj.e8707) showed increased mortality among those who substituted linoleic acid in place of saturated fats.
The second hypothesized explanation – sodium content, is similarly complex, and far from settled. This was briefly but well reviewed by Dr Alderman in a 2010 commentary (JAMA 303:448-9). Subsequently, Dr O’Donnell analyzed 2 cohorts and found a J-shaped relationship between cardiovascular events and sodium intake, with the lowest point in the curve between 3 and 7 grams of sodium intake daily (JAMA 2011, 306:2229-38).
This said, I want to congratulate Mr McClintock again for the well written post.
Ivan Saraiva, MD
Hospital das ClÃnicas, Universidade Federal de Minas Gerais, Brazil
NYU Internal Medicine Residency graduate, 2011
Comments are closed.