Peer Reviewed
Some have said that physical examination is a dying art and the nondilated funduscopic exam may be one of the best examples of this. With the increasing perception that the use of imaging and labs allows physicians to diagnose diseases with more confidence than a history and physical exam alone [1], the days when an ophthalmoscope was almost as important as the white coat or the stethoscope and was part of a “bag of tools,” are quickly becoming a distant memory [2]. One study found that the nondilated funduscopic examination using the ophthalmoscope to assess retinal vasculature was one of the physical exam skills that medical students, residents, and internists felt the least confident performing [3]. Furthermore, the study found that the same internists felt that it was the physical exam skill with the lowest perceived utility score [3]. A study in the United Kingdom found that only 56% of practitioners felt comfortable using an ophthalmoscope [4]. Therefore, with both the low perceived utility of the nondilated funduscopic exam and the lack of confidence that practitioners feel in their ability to accurately perform it, is the nondilated funduscopic exam worthwhile?
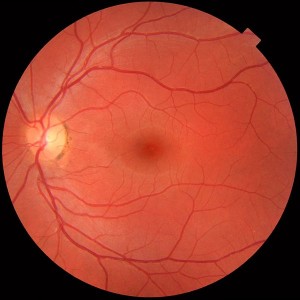
The funduscopic exam is the only part of the physical exam that offers a direct view of blood vessels as well as the central nervous system. It is also an exam of an organ that often has pathology in the general population. One study found that in a screening of a primary care population, 50% of 405 patients had ocular pathology [1]. Furthermore, some of the most common conditions such as diabetes and hypertension are associated with retinal pathology [1]. The funduscopic exam has the ability to reveal a broad range of systemic diseases, including accelerated hypertension, raised intracranial pressure, miliary tuberculosis, and cytomegalovirus [5].
The funduscopic exam can reveal pathology in a wide variety of patients:
1. Evaluating neurologic structures such as the optic disc is useful, for example in patients with headaches, evolving neurologic status, or head trauma. Papilledema or a swollen optic nerve head indicates elevated intracranial pressure. Elevated intracranial pressure is not ruled out by an absence of papilledema, as it does not occur immediately, but is less likely if retinal venous pulsations are seen on exam [6].
2. The retina may reveal proliferative changes such as those seen in immunocompromised patients. For example, Candida can cause endophthalmitis and exudates. Cytomegalovirus often leads to mixed hemorrhages and yellow granular exudates and appears like “crumbled cheese and ketchup.” Miliary tuberculosis appears with choroidal tubercles.
3. The retina can also demonstrate hemorrhages or Roth spots in patients with suspected endocarditis, pernicious anemia, leukemia, subarachnoid hemorrhage and disseminated intravascular coagulation [6]. In patients with severe hypertension, retinal hemorrhages are considered a marker of accelerated hypertension [6].
4. Pathology of vascular structures can be useful in evaluating patients with diabetes and hypertension, as diabetic retinopathy is one of the leading causes of blindness that can be contained with laser photocoagulation. Diabetic retinopathy appears as pre-proliferative lesions or frank neovascularization that leads to retinal and vitreous hemorrhage. Eventually, patients will become permanently blind if they are not treated. Furthermore, as diabetic nephropathy rarely occurs without diabetic retinopathy, the presence of proteinuria without retinopathy can indicate another underlying etiology and the need for kidney biopsy [6]. Retinal hypertension can be seen in mild systemic hypertension by generalized arteriolar narrowing and arteriovenous nicking and opacity of arteriolar walls and has been shown to predict the risk of hypertension in normotensive patients. More severe signs of hypertension, including microaneurysms, cottonwool spots, or hard exudates, are associated with a higher risk of stroke and death from cardiovascular causes [10].
5. Evidence of atheromas in peripheral blood vessels in patients with cerebrovascular disease indicates that there was a thrombotic event, as atherosclerotic plaques do not form in vessels as small as the retinal arterioles [6, 9].
Therefore, many patients with common diseases may have findings on the funduscopic examination that provide insight into their disease. While papilledema is an acute finding that is important for emergency medicine physicians to be able to assess, other pathology, like diabetic retinopathy, may be an indication for a more comprehensive exam by an ophthalmologist. Studies have shown that education can significantly improve the ability of non-ophthalmologists to detect and make appropriate referrals. One study found that after a 4-hour course, the likelihood of failing to detect and appropriately refer patients decreased from 60% to 15% in patients with preproliferative or proliferative retinopathy and decreased from 83% to 15.6% in patients with maculopathy [7]. Other studies indicate that adding retinal photographs, which allows for review by an ophthalmologist, improves the sensitivity of screening for diabetic retinopathy [8]. Furthermore, implementing retinal photographs at rural health care clinics was found to lead to an increased rate of laser therapy in diabetic patients [9].
Considering the wide range of pathology that a funduscopic examination can reveal, it is an important skill that should not be lost. Similar to other findings in the physical exam, the ophthalmologic exam should be used to obtain more information and assist the physician in forming a complete clinical picture. It should not replace the comprehensive exam by an ophthalmologist or stand in the way of digital retinal photographs, but instead should be added to the armamentarium of physical exam skills, that, combined with modern use of technology, will produce powerful and accurate physicians.
Emily Fisher is a 3rd year medical student at NYU School of Medicine
Peer reviewed by Beno Oppenheimer, MD, Medicine, NYU Langone Medical Center
Image courtesy of Wikimedia Commons : Häggström, Mikael (2014). “Medical gallery of Mikael Häggström 2014“. WikiJournal of Medicine 1 (2). DOI:10.15347/wjm/2014.008. ISSN 2002-4436. Public Domain.
References:
[1] Wang F, Ford D, Tielsch MJ, Quigley HA, Whelton PK. Undetected eye disease in a primary care clinic population. Arch Intern Med. 1994;154(16):1821-1828.
[2] Herbert F. Little black bags, ophthalmoscopy, and the Roth spot. Tex Heart Inst J. 2013; 40(2):115-116.
[3] Wu EH, Fagan MJ, Reinert SE, Diaz JA. Self-confidence in and perceived utility of the physical examination: a comparison of medical students, residents, and faculty internists. J Gen Intern Med. 2007;22(12):1725-1730.
[4] Chung KD, Wtatzke RC. A simple device for teaching direct ophthalmoscopy to primary care practitioners. Am J Ophthalmol. 2004;138(3):501-502. http://www.ncbi.nlm.nih.gov/pubmed/15364247
[5] Robertsa E, Morgana R, Kinga D, Clerkin L. Funduscopy: a forgotten art? Postgrad Med J. 1999;75:282-284.
[6] Schneiderman H. The funduscopic examination. In: Walker HK, Hall WD, Hurst JW, editors. Clinical Methods: The History, Physical, and Laboratory Examinations. 3rd edition. Boston: Butterworths; 1990. Chapter 117. Available from: http://www.ncbi.nlm.nih.gov/books/NBK221/
[7] Awh CC, Cupples HP, Javitt JC. Improved detection and referral of patients with diabetic retinopathy by primary care physicians. Effectiveness of education. Arch Intern Med. 1991;151(7):1405-1408. http://www.ncbi.nlm.nih.gov/pubmed/2064492
[8] O’Hare JP, Hopper A, Madhaven C, et al. Adding retinal photography to screening for diabetic retinopathy: a prospective study in primary care. BMJ. 1996;312(7032):679-682. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2350501/
[9] Orient JM, Sapira JD. The eye. In: Sapira’s Art & Science of Bedside Diagnosis. Philadelphia, Pa: Lippincott Williams & Wilkins; 2005:206-207.
[10] Grosso A, Veglio F, Wong TY, et al. Hypertensive retinopathy revisited: some answers, more questions. Br J Opthalmol. 2005:89(12):1646-1654. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1772998/

2 comments on “Is the Funduscopic Exam Worthwhile For the General Practitioner?”
I’d like to think that this is a useful skill as well. However, your article needs more supporting data to answer the question.
What’s the sensitivity, specificity and likelihood ratios for this test by various levels of primary care providers for important conditions?
What’s the number needed to test (NNT) for each?
Are you suggesting we should take retinal photographs in primary care as well?
The value of the funduscopic exam
The funduscopic eye exam provides clues to the patient’s developing problems in the realm of hypertension and ASVD. If the clinician can recognize arteriolar narrowing and AV niching, the early detrimental effects of hypertension and arteriolar plaque can be recognized before it becomes clinically significant. In the same way the microalbumin has become the revolutionary test for microvascular damage that is reversible for the primary care clinician, the identification of these 2 afore mentioned findings can alert the primary car clinician as to who to treat more aggressively because these findings are microvascular precursors to the macrovascular complications of HBP and ASVD. We are following guidelines for the treatment of high LDL cholesterol but many patients who have abnormal cholesterol values do not develop ASVD. AV niching will show those patients who will develop ASVD. Many patients who come in with an elevated BP have white coat hypertension but the finding of arteriolar narrowing will alert the clinician to the patient who needs close follow-up.
The optic nerve can be pushed inward with glaucoma and can be pushed forward with normal pressure hydrocephalus and malignant hypertension. The fuzzy border to the optic nerve, even a portion of it can alert the clinician to these two disorders.
The absence of venous pulsations are the first physical sign of increase intra-cranial pressure and can be a subtle finding in the patient with closed head injury, brain tumor of stroke. All the above findings are easy to identify if the clinician looks for these things on a regular basis. Once you see 100 normal eyes, the abnormal one stands out well and is easy to recognize. You can’t get good at what you don’t practice.
INTERVALIDATE on FACEBOOK
Comments are closed.