Peer Reviewed
Polypharmacy has been defined as the use of multiple unnecessary medications, the use of more medications than is clinically warranted or indicated, or the use of unnecessary, ineffective, or harmful prescribing.[1–3] Problematic polypharmacy should be differentiated from appropriate polypharmacy. Consideration of overall appropriateness of therapy is more valuable than simply considering the number of medications that an older person is prescribed.[4]
Overmedication and failure to perform prudent medication reconciliation is a growing problem in prescribing practice. In individuals over 65 years old, about 50% of the patient population takes over five prescription drugs per week, with 12% taking over ten medications per week.[5,6] The cost burden associated with adverse drug reactions is approximated to be between $37 and $50 billion.[7] Elderly patients are at increased risk of adverse drug reactions, with increased incidence associated with being prescribed a larger number of medications.[8] In the geriatric population, polypharmacy is associated with increased falls and hip fracture frequency,[10] incontinence,[11] malnutrition, and drug-drug interactions. In addition to medical complications, the pill burden of polypharmacy causes poorer adherence to prescribed medications, which can already be particularly difficult in the geriatric population, in whom cognitive impairment and memory loss are more common. Many of these adverse drug events are preventable. In the ambulatory care setting, it is estimated that 28% of adverse drug events are preventable, with 38% of the adverse events categorized as lethal or life-threatening.[12]
A range of solutions has been proposed to reduce the pharmaceutical burden and risk of adverse drug events in geriatric patients. For prescribing, physicians must take care to avoid medications with a low benefit-to-risk profile. The Beers Criteria is a guideline of drugs to avoid in geriatric patients based on risk-benefit analysis of these medications. Cardiovascular medicines, diuretics, and non-opioid analgesics were most commonly associated with adverse drug events and therefore frequently listed as drugs to avoid by the Beers criteri.12 The Screening of Older Persons’ potentially inappropriate Prescriptions (STOPP) criteria is another tool to identify potentially inappropriate medicines in geriatric patients, with more emphasis on specific clinical context. In one study, STOPP was able to identify a potentially inappropriate medicine in 35% of inpatients.[13] Medications should be prescribed in a manner to minimize prescription cascades, which can increase both the pill burden and the cumulative side effects of medications. In medication reconciliation, tools such as the Good Geriatric-Palliative Practice (GP-GP) algorithm can be applied to reduce number of medications. The GP-GP algorithm addresses each medication that a patient is taking and evaluates whether the indications are still valid at the patient’s age and whether the benefit profile outweighs the risk profile. It also explores the possibility of superior drug choice or dose changes to improve the patient’s risk profile. Using the GP-GP method in a geriatric study cohort, a study group discontinued 100% of benzodiazepines, 84% of antihypertensives, and 75% of nitrates and loop diuretics. After medication reconciliation using the GP-GP method, 86% of patients reported improvement in health with no patients having significant worsening.[14] The Assess, Review, Minimize, Optimize, Reassess (ARMOR) protocol is a systematic approach to reduce polypharmacy in the long-term care setting, but the investigators encourage its use in the outpatient setting as well. Application of the tool has not been rigorously studied, but it was associated with reduced number of medications prescribed, falls, and hospitalization in their study population.3 The Prescribing Optimization Method (POM) was developed to provide general practitioners with a rapid and easy tool to optimize prescribing in older adults in the community. Application of the POM significantly increased the frequency of appropriate drug therapy decisions made by general practitioners and improved underuse of medications.[15]
Implementation of prescribing and medication resolution guidelines can significantly improve geriatric adverse drug events, medication compliance, and morbidity and mortality. Systems-wide practice such as guideline implementation into an electronic medical record system or rounding with a pharmacist on geriatric inpatients may improve outcomes. In addition to managing prescriptions, it is important to ensure that patients have a fixed routine or assistance to take their medications as prescribed, which is difficult if patients are on medications with different dosing schedules. Medication reconciliation may also be made difficult by sparse outcomes data on the effects of discontinuing medication, as most clinical trials are designed to assess the effects of starting medication.[16] Families should know that discontinuing drugs is not providing substandard care. Consideration of polypharmacy in prescribing practice makes care more cost-effective, improves health outcomes, and is an important step in the management of every geriatric patient.
Dr. Michael Nguyen is a 3rd year medical student at NYU School of Medicine
Peer reviewed by Smitha Shetty, MD, Medicine, NYU Langone Health
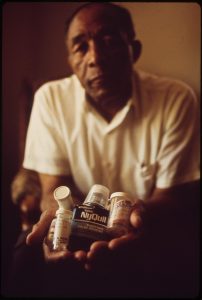
Image courtesy of Wikimedia Commons
References
1. Steinman MA. Polypharmacy–time to get beyond numbers. JAMA Intern Med. 2016;176(4):482-483. doi:10.1001/jamainternmed.2015.8597. https://www.ncbi.nlm.nih.gov/pubmed/26999383
2. Rollason V, Vogt N. Reduction of polypharmacy in the elderly: a systematic review of the role of the pharmacist. Drugs Aging. 2003;20(11):817-832.
3. Haque R. ARMOR: a tool to evaluate polypharmacy in elderly persons. Ann Long-Term Care. 2009;17(6):26–30.
4. Patterson SM, Hughes C, Kerse N, Cardwell CR, Bradley MC. Interventions to improve the appropriate use of polypharmacy for older people. Cochrane Database Syst Rev. 2012;(5):CD008165. doi:10.1002/14651858.CD008165.pub2. https://www.ncbi.nlm.nih.gov/pubmed/22592727
5. Rambhade S, Chakarborty A, Shrivastava A, Patil UK, Rambhade A. A survey on polypharmacy and use of inappropriate medications. Toxicol Int. 2012;19(1):68-73. doi:10.4103/0971-6580.94506.
6. Kaufman DW, Kelly JP, Rosenberg L, Anderson TE, Mitchell AA. Recent patterns of medication use in the ambulatory adult population of the United States: the Slone survey. JAMA. 2002;287(3):337-344.  https://www.ncbi.nlm.nih.gov/pubmed/11790213
7. Institute of Medicine (US) Committee on Quality of Health Care in America. To Err Is Human: Building a Safer Health System. Kohn LT, Corrigan JM, Donaldson MS, eds. Washington, DC: National Academies Press; 2000. http://www.ncbi.nlm.nih.gov/books/NBK225182/. Accessed January 15, 2017.
8. Col N, Fanale JE, Kronholm P. The role of medication noncompliance and adverse drug reactions in hospitalizations of the elderly. Arch Intern Med. 1990;150(4):841-845. doi:10.1001/archinte.1990.00390160093019. https://www.ncbi.nlm.nih.gov/pubmed/2327844
9. Ziere G, Dieleman JP, Hofman A, Pols HA, van der Cammen TJ, Stricker BH. Polypharmacy and falls in the middle age and elderly population. Br J Clin Pharmacol. 2006;61(2):218-223. doi:10.1111/j.1365-2125.2005.02543.x.
10. Lai SW, Liao KF, Liao CC, Muo CH, Liu CS, Sung FC. Polypharmacy correlates with increased risk for hip fracture in the elderly: a population-based study. Medicine (Baltimore). 2010;89(5):295-299. doi:10.1097/MD.0b013e3181f15efc.
11. Hogan DB. Revisiting the O complex: urinary incontinence, delirium and polypharmacy in elderly patients. CMAJ. 1997;157(8):1071-1077.
12. Gurwitz JH, Field TS, Harrold LR, et al. Incidence and preventability of adverse drug events among older persons in the ambulatory setting. JAMA. 2003;289(9):1107-1116.  https://www.ncbi.nlm.nih.gov/pubmed/12622580
13. Gallagher P, O’Mahony D. STOPP (Screening Tool of Older Persons’ potentially inappropriate Prescriptions): application to acutely ill elderly patients and comparison with Beers’ criteria. Age Ageing. 2008;37(6):673-679. doi:10.1093/ageing/afn197.  https://academic.oup.com/ageing/article/37/6/673/40813
14. Garfinkel D, Mangin D. Feasibility study of a systematic approach for discontinuation of multiple medications in older adults: addressing polypharmacy. Arch Intern Med. 2010;170(18):1648-1654. doi:10.1001/archinternmed.2010.355.  https://www.ncbi.nlm.nih.gov/pubmed/20937924
15. Drenth-van Maanen AC, van Marum RJ, Knol W, van der Linden CM, Jansen PA. Prescribing optimization method for improving prescribing in elderly patients receiving polypharmacy: results of application to case histories by general practitioners. Drugs Aging. 2009;26(8):687-701. doi:10.2165/11316400-000000000-00000.  https://www.ncbi.nlm.nih.gov/pubmed/19685934
16. Bain KT, Holmes HM, Beers MH, Maio V, Handler SM, Pauker SG. Discontinuing medications: a novel approach for revising the prescribing stage of the medication-use process. J Am Geriatr Soc. 2008;56(10):1946-1952. doi:10.1111/j.1532-5415.2008.01916.x.  https://www.ncbi.nlm.nih.gov/pubmed/18771457