 By Antonella Surbone MD PhDÂ and Jerome Lowenstein MD
By Antonella Surbone MD PhDÂ and Jerome Lowenstein MD
The recent hearings at the Food and Drug Administration regarding the revocation of approval for the use of Avastin in the treatment of breast cancer [1,2,3] bring into sharp focus several very …

 By Antonella Surbone MD PhDÂ and Jerome Lowenstein MD
By Antonella Surbone MD PhDÂ and Jerome Lowenstein MD
The recent hearings at the Food and Drug Administration regarding the revocation of approval for the use of Avastin in the treatment of breast cancer [1,2,3] bring into sharp focus several very …
 By Jonathan Leventhal
By Jonathan Leventhal
Faculty Peer Reviewed
Polypharmacy has become an integral part of daily life for millions of chronically ill patients worldwide, and rightfully so. Evidence-based studies have repeatedly demonstrated that multiple drugs are required for optimal therapeutic management in chronic diseases …
 By Joanna Becker
By Joanna Becker
Faculty Peer Reviewed
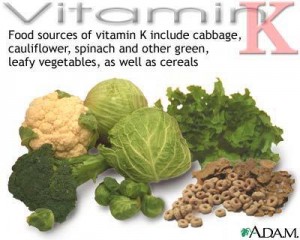
Patients who are placed on long-term warfarin (Coumadin) therapy are sent home with a lengthy list of restrictions to minimize variations in warfarin efficacy. The agents that can alter warfarin levels can be divided …
 By Saleem Ali, MD
By Saleem Ali, MD
The FDA has issued new warnings regarding the use of high dose Simvastatin. The FDA is now recommending that the 80mg dose only be used in patients who have been taking that dosage for at least …
 By Lee Rasamny
By Lee Rasamny
Faculty Peer Reviewed
For thousands of years, humans have been fascinated with the idea of slowing and perhaps even reversing the process of aging. From Ponce de León to modern …
 By Jon-Emile S Kenny
By Jon-Emile S Kenny
Faculty Peer Reviewed
A 65-year-old female with locally advanced rectal cancer is admitted to the ICU, hypotensive and febrile. Her PICC line is removed and …
 By Todd Cutler, MD
By Todd Cutler, MD
Faculty Peer Reviewed
A 62-year-old male is hospitalized with an acute congestive heart failure exacerbation. On hospital day three, the patient’s symptoms have significantly …
 By Mary C. Whitman, MD
By Mary C. Whitman, MD
Faculty Peer Reviewed
Proton pump inhibitors (PPIs) are generally considered “safe†medications[1] and are prescribed to over 100 million patients per year for a variety of indications, often …