 By Ramya Srinivasan, MD
By Ramya Srinivasan, MD
Faculty Peer Reviewed
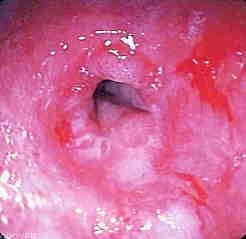
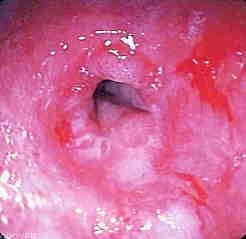
The patient is a 29 year old overweight male presenting to clinic with complaints of reflux symptoms. He says that spicy foods aggravate these symptoms. In addition …

 By Ramya Srinivasan, MD
By Ramya Srinivasan, MD
Faculty Peer Reviewed
The patient is a 29 year old overweight male presenting to clinic with complaints of reflux symptoms. He says that spicy foods aggravate these symptoms. In addition …

Introduction to Cases:
During the upcoming weeks, we will post a series of cases addressing the appropriate treatment for patients with stable coronary artery disease. We will be focus on indications for revascularization in …
 By Maura RZ Madou, MD
By Maura RZ Madou, MD
Faculty Peer Reviewed
When the New Jersey legislature approved a measure to legalize the use of marijuana for patients with chronic illnesses early this …
By Rachel Edlin, MD
Faculty peer reviewed
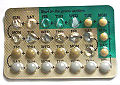
A 29-year-old female patient with a history of iron deficiency anemia and heavy menstrual periods comes into the …
 Introduction to Cases:
Introduction to Cases:
During the upcoming weeks, we will post a series of cases addressing the appropriate treatment for patients with stable coronary artery disease. We will be focus on …

Jeffrey Mayne MD
Faculty peer reviewed
Dr. Okonkwo’s post this past summer to PrimeCuts summarized ongoing research in Alzheimer’s Disease (AD), the most common cause of dementia affecting 15 …
 David Shabtai
David Shabtai
Faculty Peer Reviewed
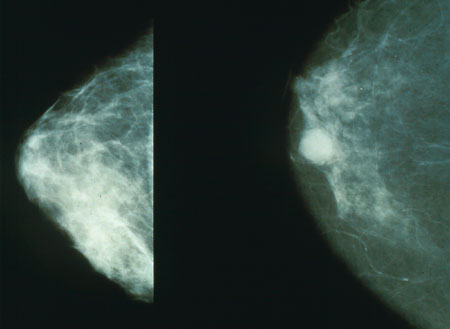
 In a bold move, the U.S. Preventive Services Task Force recently changed their breast cancer screening guidelines – recommending beginning screening at age 50 and even then only …
 Emily Stamell
Emily Stamell
Faculty peer reviewed
As a well-trained fourth year medical student, I inquire about smoking habits as part of almost all my patient encounters. Yet, I do not …