 By: Michael Moore
By: Michael Moore
Peer Reviewed
“Too many complex back surgeries are being performed and patients are suffering as a result†wrote National Public Radio health science journalist Joanne Silberner in her 2010 article “Surgery …

 By: Michael Moore
By: Michael Moore
Peer Reviewed
“Too many complex back surgeries are being performed and patients are suffering as a result†wrote National Public Radio health science journalist Joanne Silberner in her 2010 article “Surgery …
 By Carl Preiksaitis
By Carl Preiksaitis
Peer Reviewed
The term “sarcopenia†was introduced in 1989 to characterize the loss of muscle mass that occurs as a consequence of advancing age.1 Use of the term …
 By Maria Garcia-Jimenez, MD/MHS, Abinav Baweja, MD, and Nicole LaNatra, MD
By Maria Garcia-Jimenez, MD/MHS, Abinav Baweja, MD, and Nicole LaNatra, MD
Peer Reviewed
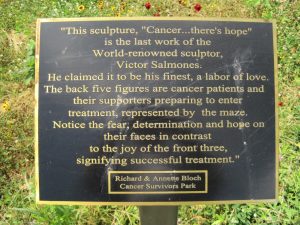
Clinical vignette
A 65-year old woman with history of invasive breast cancer presents to her primary care provider for …
 A commentary by Antonella Surbone, MD PhD FACP, Ethics Editor on yesterday’s article “Is There Such a Thing as Too Much Information?â€
A commentary by Antonella Surbone, MD PhD FACP, Ethics Editor on yesterday’s article “Is There Such a Thing as Too Much Information?â€
The insighftul and challenging piece Is there such a …
 Aalok Turakhia MD
Aalok Turakhia MD
In an attempt to err on the side of safety, an advisory panel to the Federal Food and Drug Administration narrowly voted yesterday to ban the popular …
 Commentary by Albert B. Knapp MD, NYU Clinical Professor of Medicine (Gastroenterology)
Commentary by Albert B. Knapp MD, NYU Clinical Professor of Medicine (Gastroenterology)
THE CASE:
WS, a 49 yo year old Caucasian male with a known 35 year history of alcohol abuse, now presents …
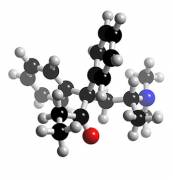 Last week, the FDA issued a public health advisory regarding the use of methadone (trade name Dolophine) for chronic pain. Death and life threatening side effects have been reported in patients …
Last week, the FDA issued a public health advisory regarding the use of methadone (trade name Dolophine) for chronic pain. Death and life threatening side effects have been reported in patients …