 By Elana Kreiger-Benson
By Elana Kreiger-Benson
Peer Reviewed
“I’m not actually planning to try it,†the patient whispered to me while I was feeling her radial pulses. We had just finished an extensive conversation with her primary care …

 By Elana Kreiger-Benson
By Elana Kreiger-Benson
Peer Reviewed
“I’m not actually planning to try it,†the patient whispered to me while I was feeling her radial pulses. We had just finished an extensive conversation with her primary care …
 By Lily Cao
By Lily Cao
Peer ReviewedÂ
A quick web search would suggest countless reasons to take fish oil, a supplement that Americans have fallen in love with. In 2012, …
 By Ashira Lubkin, PhD
By Ashira Lubkin, PhD
Peer Reviewed
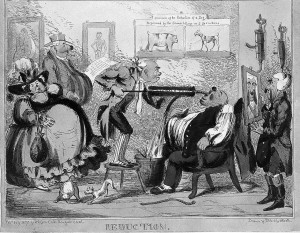
For me, one of the most difficult things to do in outpatient medicine is to tell a patient that they need to lose …
 By Hannah Kopinski
By Hannah Kopinski
Peer Reviewed
Diabetes, hypertension, and hyperlipidemia. One would be hard pressed to find an adult primary care physician in the United States who would not …
 By Andrew Sideris
By Andrew Sideris
Peer Reviewed
Reduction of dietary sodium is a well-known nonpharmacologic therapy to reduce blood pressure. The 8th Joint National Commission (JNC-8) recommends that the general population limit daily …
 By Elissa Driggin
By Elissa Driggin
Peer Reviewed
At almost every single one of my medical school interviews, each interviewer, noting my college major in nutritional science, asked some variation of the question, “What …
Please enjoy this post from the archives dated September 30, 2011
 By Vicky Jones, MD
By Vicky Jones, MD
A 40-year-old female presented to her primary care provider with a chief complaint of weight gain over the past year. She wants to be fully evaluated for any …
 By Michael Lee, MD
By Michael Lee, MD
Peer Reviewed
The human taste bud has become increasingly accustomed to the Japanese invention of the early 20th century: monosodium glutamate, better known as MSG. Its basic component, …