 By Emily Lock
By Emily Lock
Peer Reviewed
Sleep is a currency of wellness. Increased sleep duration has been associated with enhanced cognitive performance and decreased risk …

 By Emily Lock
By Emily Lock
Peer Reviewed
Sleep is a currency of wellness. Increased sleep duration has been associated with enhanced cognitive performance and decreased risk …
 By Alvaro Vargas, MD
By Alvaro Vargas, MD
Peer ReviewedÂ
Learning Objectives
 By Gregory Rubinfeld, MD
By Gregory Rubinfeld, MD
Peer Reviewed
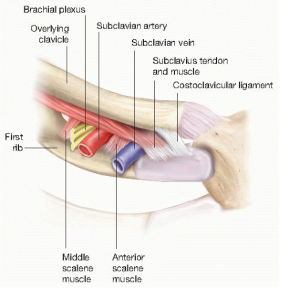
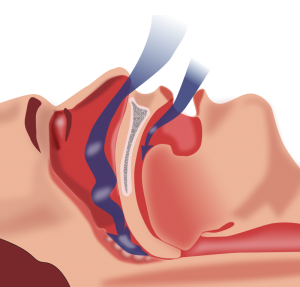
Obstructive sleep apnea (OSA) is an increasingly prevalent disorder that has well described associations with cardiovascular disease. OSA affects approximately 20–30% of males and 10–15% of females in North America.1-3 In addition to male gender, other risk …
 By Rebecca Lazarus, MD
By Rebecca Lazarus, MD
Peer Reviewed
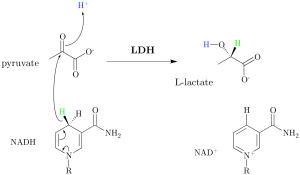
The concept of lactate is frequently on the tip of the tongue or top of the to-do list in the hospital setting. …
 By Jasmine Nee and Martin Fried, MD
By Jasmine Nee and Martin Fried, MD
Peer Reviewed
LEARNING OBJECTIVES
1. What is metformin-associated lactic acidosis?
2. How does severe acidemia lead to acute kidney injury?
3. How do you treat metformin-associated lactic …
 By Scott Statman, MD
By Scott Statman, MD
Peer Reviewed
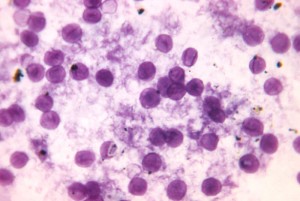
There is little doubt that an association between asthma and gastroesophageal reflux disease (GERD) exists. However clinicians have debated the nature of this relationship for decades. Asthma and …
 By Martin Fried, MD
By Martin Fried, MD
Peer reviewed
Learning Objectives
 By Christopher V. Cosgriff
By Christopher V. Cosgriff
Peer Reviewed
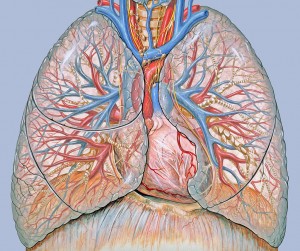
The American College of Physicians (ACP) recommends supplemental long-term oxygen therapy (LTOT) in all patients who have severe resting hypoxemia, defined as a PaO2 ≤55 mmHg …